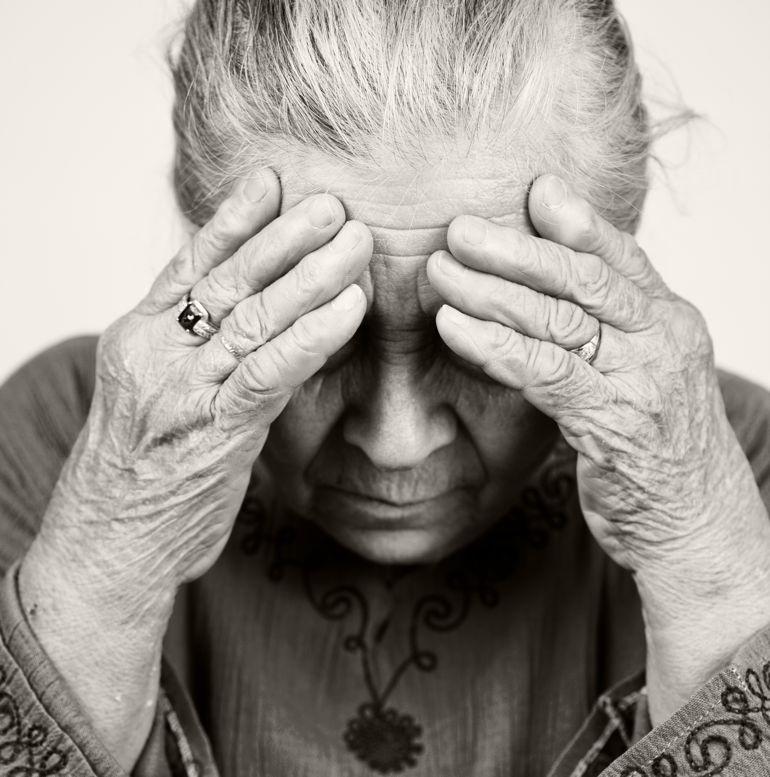
Just hearing the doctor say the word "cancer" can have a profound effect on a person. A diagnosis of cancer begins a long journey that can affect physical health, mental well-being, and relationships with loved ones. While getting treatment for the physical aspects of cancer, patients should not neglect the emotional issues associated with cancer. One of the best things patients can do to improve their quality of life is to learn more about their cancer. This can make the disease seem less mysterious and frightening. Information from your doctor and other credible sources can be very helpful in this respect.
A patient's financial, social and physiological situations may all change due to cancer and cancer treatment. Having a realistic attitude and realizing that cancer can impact many aspects of life is helpful. Patients should not be afraid to tell their doctor how they are feeling, especially when it involves worries. Studies have shown that cancer care doctors misinterpret a patient distress or psychological disorders as much as 35% of the time. 1, 2For this reason, it is important to tell your doctor about any pain and feelings of anxiety or despair. Some people feel uncomfortable accepting psychological help because they feel it is only for weak or irrational people. The brain is like any other organ; illnesses in other parts of the body can affect the brain and impact the well-being of the individual. It is important to seek help from a medical professional when there are changes that cause discomfort or unhappiness.
- Social Support Network
- Relationships
- Intimacy, Body Image
- Anxiety
- Depression
- Self Assessment Test for Depression
- Uncertainty and Negativity
- Anger and Fear
- Additional Resources
Watch the full interview with Dr. Michael Burke, a psychiatric oncologist
Social Support Network
Introduction
People in a patient's social support network include family members, spouses, children and friends. Social support can also take the form of support groups or therapists.3 It is important for these caregivers to listen to the unique needs and concerns of their loved one. For instance, they should be sensitive to the desire of the patient to share and know information about their cancer, treatment options, and their prognosis.3 A support network can greatly help reduce the stress of dealing with cancer. Patients should not be afraid to ask for help from loved ones and friends. The people in a patient's support network can help ensure that they get to appointments on time, pick up children or just be there to listen to the patient's concerns.4
Importance
A lack of social support has been associated with higher levels of anxiety and a lower quality of life in cancer patients. 5, 6A lower incidence of depression is associated with the ability of family members to openly express feelings and thoughts to the patient. Anxiety is also less common when patients are able to freely communicate information to their family members.7 Most importantly, cancer patients who have a lack of social support have a greater desire to die and a higher risk of committing suicide.8, 9
Treatment
A good social support network has been linked with an increased quality of life for cancer patients undergoing treatment.3 Information about cancer can also make the patient feel more empowered, giving them a sense of control. Nearly all studies have shown a psychological benefit for cancer patients who attend support groups.10, 11 Most patients attending support groups feel more emotionally fulfilled, get help managing side effects and experience less pain and anxiety.12 Support group attendance may also extend the life of cancer patients, but more investigation is needed to verify this.13, 14
Click here to watch the full interview with Dr. Michael Burke, a psychiatric oncologist.
Having cancer may change the way that a patient relates with family, friends, and colleagues. Patients may find that the stress going through a cancer diagnosis and treatment strengthens their relationships with loved ones. While some relationships provide much needed support, other relationships may unexpectedly lead to frustration. In many cases, stress in the relationship is caused by misunderstandings and confusion of how to offer support to a cancer survivor. Many want to offer support, but they just do not know how. With open communication, these issues may be resolved.
After treatment ends, some friends, family, or coworkers may appear to show less support due to their belief that the cancer is gone. They may seem unsupportive due to anxiety and other emotions; speaking with that friend, family member, or coworker can help to mend and strengthen relationships. As survivors work through relationships to figure out what matters most in their life, some may choose to let some casual friendships go as they focus more on those that are more valuable and meaningful.
In addition to dealing with their own feelings, a cancer survivor may also have to cope with their friends and families feelings of sadness and uncertainty. Everyone needs recovery time, both the cancer survivor and those close to them.
Family members and friends of different ages face different challenges. For example, young children may convince themselves that they were somehow to blame for the cancer. Teenagers, on the other hand, may find it difficult to cope because they may feel they have been forced back into the family just as they were beginning to break free and gain their independence. Remember that silence can block communication and that open communication is critical to maintain healthy relationships.

Introduction
People undergoing cancer treatment may lose their hair, experience weight changes, get surgical scars or have body parts surgically altered/removed. It is normal for these events to change a person's sex drive and body image. Cancer/cancer treatments affecting reproductive organs (breast, prostate, testicles, etc.) may cause patients to question their social and sexual identity as a 'man' or 'woman'. 15, 16This is true for people of all ages, genders, cultures, cancer types, and is independent of partnership status. 15Because doctors may not discuss this issue, patients may incorrectly feel they are abnormal to be concerned about their sexuality and sex life. 17
In fact, most people going through cancer treatment feel that their needs and concerns about sexual and intimate changes are not adequately met by their health care professionals. 15Doctors trained in traditional Western medical schools learn ways to handle the functional aspects of patient sexuality such as fertility, erectile dysfunction, or menopause. Frequently, their training does not prepare them to provide guidance about sensuality and intimacy issues. 16Doctors often avoid the topic of intimacy because it is not a 'life or death' issue, there is not enough time, they themselves are embarrassed about the topic, or they do not have experience in this area. 18, 19, 20Some health professionals also struggle to accept the fact that people with life-threatening illnesses, particularly elderly people, have sexual concerns.21
Importance
Desire for survival can take precedence over other concerns when people are first diagnosed with a life-threatening disease like cancer. 22Cancer patients may lose interest in sex and even though few talk about it, this is quite normal. Over time, patients may wish to 'get on with life' and return to normal activities. 22Sexuality can be important to a person's identity and a change in body image can affect intimate and social relationships. 22Intimacy with a partner can also be an important way to communicate, alleviate suffering and retain a sense of self.21, 22
Treatment
It may take time and patience to adjust to fatigue, altered sensations, or prostheses. Patients should speak with their health care professionals about any concerns or questions they may have.22 Unfortunately, there has not been much research about how to best deal with changes in sexuality, body image and intimacy related to cancer.16
Click here for frequently asked questions about breast reconstruction surgery risks, benefits, and options.
Anxiety
Introduction
Anxiety is a normal reaction to a cancer diagnosis. When people feel threatened, their stress level naturally goes up. Cancer can be very dangerous and so many patients become anxious. 23Symptoms include shaking, fast or irregular heartbeat, and extreme levels of worry. Anxiety can occur at any and all times during caner screening, diagnosis, and treatment. 23About 48% of cancer patients report high levels of anxiety and 18% experience anxiety disorders.6
Watch the video and find how lung cancer survivor Edward Levitt deals with the stress of living with cancer.
Importance
Patients who are unmarried and undergoing treatment are at a higher risk of suffering from anxiety. 5People who have anxiety at the time of diagnosis, severe pain, lack of social support, advancing disease, and previous anxiety disorders are also at high risk to develop anxiety disorders during treatment. <6, 24 The fears associated with anxiety may cause enough mental suffering to prevent patients from performing activities normally. 6Anxiety can interfere with a patients quality of life and the ability to follow through with their cancer therapy. 23Higher levels of insomnia, pain expectation, and depression may also be a result of anxiety.23, 6
Treatment
A patient can alleviate anxiety by learning more about their cancer, though psychological interventions and with the help of drugs. In cases in which anxiety is caused by pain, a hormone producing tumor, or side effects from medication, treating the source can relieve anxiety.25
Click here to watch the entire interview with Ed Levitt.
Depression
Introduction
Depression can be a very important mental issue for cancer patients. It is estimated that 16-25% of cancer patients develop depression. 26, 27Doctors do not recognize about 35% of these cases and many patients remain untreated. 28Depression is also more common in cancer patients than the general population. 29There are several categories of depression with major depression being the most noticeable type. Major depression is defined as at least five of the following symptoms for two weeks or more:30
- Depressed mood lasting for most of the day, nearly everyday
- Noticable loss of pleasure or interest in normal activities for most of the day, nearly everyday
- Significant weight loss/gain and decrease/increase in appetite
- Sleeping much more than usual or much less than usual
- Fatigue or loss of energy nearly everyday
- Feelings of worthlessness or inappropriate guilt
- Decreased ability to think or concentrate
- Frequent thoughts of death or suicide
Watch the entire interview with Tony LaRocco.
Cancer can alter a patient's life plans, body image, family/social role and financial status. It is normal to fear these changes but this fear usually lessens over several days or weeks as people adjust to the diagnosis 31. Depression can have different effects on each individual and patients with a more advanced disease are more likely to be depressed. It is normal to have feelings of grief and sadness but it is important for cancer patients to distinguish between normal degrees of grief and depressive disorders. 32
Below is a table highlighting some differences between grief and depression.31
Characteristics of Grief | Characteristics of Depression |
| Patients experience somatic distress, loss of usual patterns of behavior, agitation, sleep and appetite disturbances, decreased concentration, social withdrawal | Patients experience similar symptoms, plus hopelessness, helplessness, worthlessness, guilt, and suicidal thoughts |
| Grief is associated with disease progression | Depression has an increased prevalence (up to 77%) in patients with advanced disease; pain is a major risk factor |
| Patients retain the capacity for pleasure | Patients enjoy nothing |
| Grief comes in waves | Depression is constant |
| Patients express passive wishes for death to come quickly | Patients express intense and persistent suicidal thoughts |
| Patients are able to look forward to the future | Patients have no sense of a positive future |
Importance
Current depression, poorly controlled pain, advanced stage cancer, a lack of family support and diagnosis with particular cancer types (i.e. pancreatic cancer) are all associated with an increased risk of depression in cancer patients. 33, 34, 35Causes of depression include:
- Psychological stress
- Biological problems
- Side effect of medication
- Reaction to chemotherapy36
- Dysfunctional thyroid gland
- Inadequate diet
Studies have shown that if depression goes untreated it can have negative effects on other health issues. 37, 38, 39Depression can make it difficult for patients to make decisions about treatments, slow recovery, and increase a patient's risk of dying. 33, 40Older patients and women tend to suffer from cancer related depression more than younger patients and men, respectively. 5Breast cancer patients with depression do not live as long other breast cancer patients. 41, 42 A study of renal cancer patients showed that those with depression had reduced survival. The authors of the study linked depression with changes in the inflammatory responses in the patients.43 Depression is also important to avoid because it is recognized as a major risk factor for suicide.44
Treatment
There are two distinct types of treatment for depression: psychotherapy and pharmacotherapy. In psychotherapy, patients are helped to deal with their emotions and worrisome thoughts. This type of intervention can include counseling, relaxation techniques, cancer education, hypnosis, and support groups.
Pharmacotherapy involves the use of prescription antidepressants. This aspect of treatment deals with the chemical and biological aspect of the brain. Studies have shown that the best way to treat cancer related depression is with both pharmacotherapy and psychotherapy.45, 46
NOTE: These are general guidelines not medical advice. If you or a loved one believes they may be depressed you should contact a licensed health professional.
Self Assessment Test for Depression
The Center for Epidemiological Studies - Depression Scale is a self-report scale developed to assess a patients signs of depression. It was developed in 1977 by Lenor Radloff and is regularly used by mental health professionals.47 Its accuracy has been validated for cancer patients since its inception.48
To take the test: read the instructions and click on one circle per line. Take your time and try to be as honest. When you are done click on the "Score" button to receive your results. Below is a general assessment of results.This test is anonymous and no information will be recorded.
This is simply a preliminary assessment tool and it does not provide a complete and accurate diagnosis. If you feel you need help, please seek the advice of a physician or health professional regardless of the outcome of this test. Getting help is not a sign of weakness; depression is a medical illness that can commonly affect people with cancer.
CES-D Self Test
Instructions: Read the list of ways you may have felt. Please indicate how often you have felt this way during the past week: rarely or none of the time, some or a little of the time, occationally or a moderate amount of time, or most or all of the time.
| During the past week, that would be from last Monday through today: | Rarely or none of the time (less than 1 day) | Some or a little of the time (1-2 days) | Occasionally or a Moderate Amount of Time (3-4 days) | Most or all of the time (5-7 days) |
|---|---|---|---|---|
| 1. You were bothered by things that usually don't bother you. | ||||
| 2. You did not feel like eating anything; your appetite was poor. | ||||
| 3. You felt that you could not shake off the blues even with help from your family or friends. | ||||
| 4. You felt that you were just as good as other people. | ||||
| 5. You had trouble keeping your mind on what you were doing. | ||||
| 6. You felt depressed. | ||||
| 7. You felt that everything you did was an effort. | ||||
| 8. You felt hopeful about the future. | ||||
| 9. You thought your life had been a failure. | ||||
| 10. You felt fearful. | ||||
| 11. Your sleep was restless. | ||||
| 12. You were happy. | ||||
| 13. You talked less than usual. | ||||
| 14. You felt lonely. | ||||
| 15. People were unfriendly. | ||||
| 16. You enjoyed life. | ||||
| 17. You had crying spells. | ||||
| 18. You felt sad. | ||||
| 19. You felt that people disliked you. | ||||
| 20. You could not get "going". |
Scoring and Assessment
Less than 16 Depression is not indicated
Consult a social worker to address any concerns you may have. People with scores in this range usually do not have clinical depression. However, emotional distress can be common in people with cancer. You are encouraged to get assistance from friends, family, clergy, social worker or your primary health care team.
16 - 20 Mild depression indicated
Seek assistance from mental health professional and/or a physician. People with scores in this range usually have a mild clinical depression that should be addressed. Getting help is not a sign of weakness; depression is a medical illness that can commonly affect people with cancer.
21-25 Moderate depression indicated
Seek assistance from mental health professional and/or a physician. People with scores in this range usually have a moderate clinical depression that should be addressed. Getting help is not a sign of weakness; depression is a medical illness that can commonly affect people with cancer.
26 or higher Severe depression indicated
It is important that you get assistance as soon as possible from your physician or mental health professional. People with scores in this range usually have a severe clinical depression. Getting help is not a sign of weakness; depression is a medical illness that can commonly affect people with cancer.
Getting Help
Special thanks to Dr. Andy Miller and Dr. Michael Burke.
Uncertainty and Negativity
It is common that a survivor may feel uncertainty in planning the future because they are not sure what will happen in terms of their cancer treatment. If a cancer survivor experiences negative feelings, it is important to remember that everyone has low times and that acknowledging and recognizing feelings of tiredness, anxiety, anger, and depression is actually a positive thing. Expressing feelings openly and honestly can often help to relieve stress and tension. Strong feelings ranging from self-blame, need to blame others, overwhelming stress, and guilt may be frightening but are common.

Anger is a natural reaction to the loss of normalcy that may accompany a cancer diagnosis. It is likely that friends and family are feeling the same emotions. When strong feelings like anger are held in, problems such as depression, tiredness, hopelessness, and a lack of motivation can develop. It is very important to release these feelings by speaking with friends, family, or a licensed healthcare professional.
Resources for Psychosocial Effects
- 1 Fallowfield L, Ratcliffe D, Jenkins V, Saul J. Psychiatric morbidity and its recognition by doctors in patients with cancer. Br J Cancer. (2001) 84(8):1011-5. [PUBMED]
- 2 Keller M, Sommerfeldt S, Fischer C, Knight L, Riesbeck M, Löwe B, Herfarth C, Lehnert T. Recognition of distress and psychiatric morbidity in cancer patients: a multi-method approach. Ann Oncol. (2004) 15(8): 1243-9 [PUBMED]
- 3abc Ludwig H, Zojer N. Supportive care. Ann Oncol. 2007 Jan;18 Suppl 1:37-i44. [PUBMED]
- 4 The National Cancer Institute. When Someone You Love is Being Treated for Cancer. U.S. National Institutes of Health. Accessed Aug. 8, 2007. Web site: [http://www.cancer.gov/cancertopics/When-Someone-You-Love-Is-Treated]
- 5abc Mystakidou K, Tsilika E, Parpa E, Katsouda E, Galanos A, Vlahos L. Assessment of anxiety and depression in advanced cancer patients and their relationship with quality of life. Qual Life Res. (2005) 14(8):1825-33 [PUBMED]
- 6abcde Stark D, Kiely M, Smith A, et al. Anxiety disorders in cancer patients: their nature, associations, and relation to quality of life. J Clin Oncol (2002) 20(14): 3137-48 [PUBMED]
- 7 Edwards B, Clark V. "The psychological impact of a cancer diagnosis on families: the influence of family functioning and patients' illness characteristics on depression and anxiety." Psychooncology (2004) 13(8): 562-76. [http://www.ncbi.nlm.nih.gov/pubmed/15295777?dopt=Abstract] [PUBMED]
- 8 Breitbart W, Chochinov HM, Passik SD. Psychiatric symptoms in palliative medicine. In: Doyle D, Hanks G, Cherny N, Calman K (eds). The Oxford textbook of palliative medicine, 3rd edn. Oxford: Oxford University Press, 2004:74671.
- 9 Breitbart W, Rosenfeld B, Pessin H, et al. Depression, hopelessness, and desire for hastened death in terminally ill patients with cancer. JAMA. (2000) 284(22): 2907-11 [PUBMED]
- 10 Goodwin PJ. Support groups in advanced breast cancer. Cancer. (2005) 104(11): 2596-601 [PUBMED]
- 11 Carmack Taylor CL, Kulik J, Badr H, Smith M, Basen-Engquist K, Penedo F, Gritz ER. A social comparison theory analysis of group composition and efficacy of cancer support group programs. Soc Sci Med. (2007) Apr 18; [PUBMED]
- 12 Jones LW, Demark-Wahnefried W. Diet, exercise, and complementary therapies after primary treatment for cancer. Lancet Oncol. (2006) 7(12): 1017-26 [PUBMED]
- 13 Fawzy FI, Canada AL, Fawzy, NW. Malignant melanoma: effects of a brief, structured psychiatric intervention on survival and recurrence at 10-year follow-up. Arch Gen Psychiatry. (2003) 60(1): 100-3 [PUBMED]
- 14 Weis J. Support groups for cancer patients. Support Care Cancer. (2003) 11: 763-8. [PUBMED]
- 15abc Hordern AJ, Street AF. Communicating about patient sexuality and intimacy after cancer: mismatched expectations and unmet needs. Med J Aust. 2007 186(5): 224-7 [PUBMED]
- 16abc Hordern AJ, Street AF. Constructions of sexuality and intimacy after cancer: patient and health professional perspectives. Soc Sci Med. 2007 Apr;64(8):1704-18. Epub 2007 Jan 29 [PUBMED]
- 17 Wilmoth MC. The aftermath of breast cancer: an altered sexual self. Cancer Nurs 2001; 24: 278-286 [PUBMED]
- 18 Stead, M. L., Brown, J. M., Fallowfield, L., & Selby, P. (2002). Communication about sexual problems and sexual concerns in ovarian cancer: A qualitative study. Western Journal of Medicine, 176(1), 1819 [PUBMED]
- 19 Stead, M. L., Brown, J. M., Fallowfield, L., & Selby, P. (2003). Lack of communication between healthcare professionals and women with ovarian cancer about sexual issues. British Journal of Cancer, 88, 666671. [PUBMED]
- 20 Lemieux L, Kaiser S, Pereira J, Meadows L. Sexuality in palliative care: patient perspectives. Palliat Med 2004; 18: 630-637 [PUBMED]
- 21ab Hordern A, Currow D. A patient-centred approach to sexuality in the face of life-limiting illness. Med J Aust 2003 179 (6 Suppl): 8-11 [PUBMED]
- 22abcde Hordern A. Intimacy and sexuality for the woman with breast cancer. Cancer Nurs 2000; 23: 230-236 [PUBMED]
- 23abcd Mystakidou K, Tsilika E, Parpa E, Katsouda E, Galanos A, Vlahos L. Psychological distress of patients with advanced cancer: influence and contribution of pain severity and pain interference. Cancer Nurs. (2006) (5):400-5 [PUBMED]
- 24 Green BL, Krupnick JL, Rowland JH, et al.: Trauma history as a predictor of psychologic symptoms in women with breast cancer. J Clin Oncol (2000) 18(5): 1084-93. [PUBMED]
- 25 Montazeri A, Jarvandi S, Haghighat S, et al.: Anxiety and depression in breast cancer patients before and after participation in a cancer support group. Patient Educ Couns (2001) 45(3): 195-8 [PUBMED]
- 26 Patrick DL, Ferketich SL, Frame PS, Harris JJ, Hendricks CB, Levin B, Link MP, Lustig C, McLaughlin J, Ried LD, Turrisi AT 3rd, Unutzer J, Vernon SW; National Institutes of Health State-of-the-Science Panel. National Institutes of Health State-of-the-Science Conference Statement: Symptom Management in Cancer: Pain, Depression, and Fatigue, (2002) J Natl Cancer Inst. 2003 Aug 6;95(15):1110-7 [PUBMED]
- 27 Fisch MJ, Callahan CM, Kesterson JG, et al.: The use of an electronic patient record system to identify advanced cancer patients and antidepressant drug use. J Palliat Med (1999) 2 (4): 403-9. [PUBMED]
- 28 Bottomley A (1998) Depression in cancer patients: a literature review. Eur J Cancer Care 7(3):181191 [PUBMED]
- 29 Massie MJ. Prevalence of depression in patients with cancer. J Natl Cancer Inst Monogr 2004;(32):57-71 [PUBMED]
- 30 American Psychiatric Association. (1994). Diagnostic and statistical manual of mental disorders (4th ed.). Washington, DC: American Psychiatric Association.
- 31ab Block SD. Assessing and Managing Depression in the Terminally Ill Patient. Annals of Internal Medicine. (2000) 132(3); 209-218. [PUBMED]
- 32 Rodin G, Lloyd N, Katz M, Green E, Mackay JA, Wong RK; Supportive Care Guidelines Group of Cancer Care Ontario Program in Evidence-Based Care. The treatment of depression in cancer patients: a systematic review. Support Care Cancer. 2007 Feb;15(2):123-36. Epub 2006 Oct 21 [PUBMED]
- 33ab Nordin K, Glimelius B: Predicting delayed anxiety and depression in patients with gastrointestinal cancer. Br J Cancer (1999) 79(3-4): 525-9 [PUBMED]
- 34 Karnell LH, Funk GF, Christensen AJ, et al.: Persistent posttreatment depressive symptoms in patients with head and neck cancer. Head Neck (2006) 28 (5): 453-61 [PUBMED]
- 35 Ciaramella A, Poli P: Assessment of depression among cancer patients: the role of pain, cancer type and treatment. Psychooncology (2001) 10 (2): 156-65 [PUBMED]
- 36 Capuron L, Ravaud A, Gualde N, et al.: Association between immune activation and early depressive symptoms in cancer patients treated with interleukin-2-based therapy. Psychoneuroendocrinology. (2001) 26 (8): 797-808 [PUBMED]
- 37 House A, Knapp P, Bamford J, Vail A. Mortality at 12 and 24 months after stroke may be associated with depressive symptoms at 1 month. Stroke. 2001 Mar;32(3):696-701 [PUBMED]
- 38 Watson M, Haviland JS, Greer S, Davidson J, Bliss JM. Influence of psychological response on survival in breast cancer: a population-based cohort study. Lancet. 1999 Oct 16;354(9187):1331-6. [PUBMED]
- 39 Glassman AH, OConnor CM, Califf RM, et al. Sertraline treatment of major depression in patients with acute MI or unstable angina. JAMA. (2002) 288(6): 701-9. [PUBMED]
- 40 Stommel M, Given BA, Given CW. Depression and functional status as predictors of death among cancer patients. Cancer (2002) 94: 27192727. [PUBMED]
- 41 Goodwin JS, Zhang DD, Ostir GV. Effect of depression on diagnosis, treatment, and survival of older women with breast cancer. J Am Geriatr Soc 2004;52:106-11. [PUBMED]
- 42 Spiegel D, Bloom JR, Kraemer HC, Gottheil E. Effect of psychosocial treatment on survival of patients with metastatic breast cancer. Lancet. (1989) 2(8668): 888-91 [PUBMED]
- 43 Lorenzo Cohen, Steven W. Cole, Anil K. Sood, Sarah Prinsloo, Clemens Kirschbaum, Jesusa M. G. Arevalo, Nicholas B. Jennings, Shellie Scott, Luis Vence, Qi Wei, Diane Kentor, Laszlo Radvanyi, Nizar Tannir, Eric Jonasch, Pheroze Tamboli, Louis Pisters. Depressive Symptoms and Cortisol Rhythmicity Predict Survival in Patients with Renal Cell Carcinoma: Role of Inflammatory Signaling. (2012) PLoS ONE 7(8): e42324. doi:10.1371/journal.pone.0042324 [http://www.plosone.org/article/info%3Adoi%2F10.1371%2Fjournal.pone.0042324]
- 44 Cathcart F. Psychological distress in patients with advanced cancer. Clin Med. 2006 Mar-Apr;6(2):148-50. Review. No abstract available [PUBMED]
- 45 Keller MB, McCullough JP, Klein DN, Arnow B, Dunner DL, Gelenberg AJ et al A comparison of nefazodone, the cognitive behavioral-analysis system of psychotherapy, and their combination for the treatment of chronic depression. N Engl J Med. (2000) 342 (20): 14621470 [PUBMED]
- 46 Thase ME. Psychotherapy of refractory depressions. Depress Anxiety (1997) 5(4): 190201 [PUBMED]
- 47 Lenore Radloff. The CES-D Scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977; 1: 385. [http://apm.sagepub.com/cgi/content/abstract/1/3/385]
- 48 D Hann, K Winter, P Jacobsoen. Measurement of depressive symptoms in cancer patients: Evaluation of the Center for Epidemiological Studies Depression Scale (CES-D). Journal of Psychosomatic Research. 199; 46: 437-443. [PUBMED]
- 49 Patient Resource. Cancer Survivorship: A Guide for Patients and Their Families. Pg 18-22. 2014.[PATIENT RESOURCE]
