Introduction
Since the 1940s, scientists have isolated compounds and tested their ability to induce cancer. Substances which can cause cancer are known as carcinogen and the process of cancer development is called carcinogenesis. It was suspected early-on that carcinogens caused cancer indirectly, by causing DNA mutations. One early observation supporting this was that X-rays, which were shown to damage DNA, can cause cancer. Since then, other types of radiation, many chemicals and some bacteria and viruses have been shown to cause cancer.
Cancer cells do not look or act like the normal cells from which they originate. It is reasonable, then, to ask 'Why do cancer cells behave so badly?'. It turns out the the answers lie in the genes of the affected cells. In cancer cells, changes to key genes cause the cells to act abnormally. The changes are often the result of changes to the DNA (mutations) in the cells. Because there are many different things that are capable of causing mutation, there are an equally large number of causes of cancer. Further information on the topics on this page can also be found in most introductory Biology textbooks, we recommend Campbell Biology, 11th edition.1
Below is a list of topics covered in this section:
- Environmental Agents and Cancer Development
- Infections that Cause Cancer
- Obesity and Cancer
- Chronic Inflammation and Cancer Development
- Detecting Carcinogens: The Ames Test
- List of Carcinogens and the Cancers They Cause
- Tobacco
- Alcohol
Environmental Agents and Cancer Development
Environmental Exposure
Population (epidemiological) and laboratory studies have led to the discovery of many potential environmental factors in the initiation, promotion and progression of cancer. Starting with Pott's observations in the 18th century, certain occupations have been associated with an increased risk of cancer development. The recognition of increased scrotal cancer in chimney sweeps due to coal and tar exposure was followed by an observation in a British factory that all men distilling 2-napthylamine developed bladder cancer. 2 Nickel refining, leather working and woodworking have also been associated with an increased risk of specific cancers due to chronic exposure to carcinogenic chemicals. Exposure to mustard gas, used as a chemical warfare agent in World War I has been associated with a higher risk of respiratory tract and lung cancers due to its mutagenic properties.3 Of interest, some chemotherapy drugs are derivatives of mustard gas and are useful for the very same reason; they are highly mutagenic.
Geographical Influences
There have also been associations made between different geographical regions and particular cancers. Stomach cancer is 5-6 times higher among Japanese men, attributed to the consumption of fermented foods; breast cancer is 20 times higher among American women, attributed to the high fat American diet; and liver cancer is 10 times higher in Africa, which correlates with high rates of Hepatitis B infection. 4 Liver cancer may also be caused by aflatoxin, a food contaminant produced by fungi. This compound is prevalent in grain stores in tropical and subtropical regions because moist grain is a very good place for the fungi to live. 5
Lifestyle
The impact of many environmental factors can be reduced by making healthy lifestyle choices. Some examples include:
- Cigarettes: One of the most potent human carcinogens is benzo[a]-pyrene, a compound found in cigarette smoke. 2 In fact, the tar in cigarette smoke includes both initiators and promoters, making it especially dangerous. Alcohol is a promoter of carcinogenesis in humans, as is asbestos.
- Hair dyes and straighteners: In 2019, results from a large study showed that regular use of hair dyes and hair straighteners was linked to an increase in breast cancer in women.6
- UV radiation: Radiation from the sun or tanning beds, is a powerful mutagen and cancer causing agent in humans and is a major cause of skin cancer. 4
See our detailed section on tobacco and cancer.
Drugs
Tamoxifen, a chemotherapeutic agent used to combat estrogen receptor positive (ER+) breast cancer, increases the risk of endometrial cancer by increasing the rate of endometrial cell proliferation. For this reason, long-term tamoxifen treatment is losing popularity in favor of aromatase inhibitors.7 Estrogens themselves may also be important in the promotion of tumors, particularly in post-menopausal women receiving exogenous estrogens, due to their ability to increase mammary and endometrial cell division rates.8 This is an area of active research.
There are factors that can predispose an unborn fetus to developing cancer later in life. These include exposure to radiation or the synthetic estrogen diethylstilbestrol (DES).9
A Closer Look at Aflatoxin: Physical Impact and Associated Cancer
Exposure: Aflatoxin is produced by Aspergillus flavus and Aspergillus parasiticus fungi. The fungi synthesize aflatoxin when they are living in warm, moist conditions. These fungi are prevalent among crops such as rice, corn, cassava, nuts, peanuts, chilies, and spices. Countries with the highest amounts of these organisms lie within 40 degrees latitude north or south of the equator. Storage of food under warm, moist conditions increases the risk of aflatoxin contamination. Approximately 4.5 billion persons living in developing countries are chronically exposed to uncontrolled amounts of aflatoxin.10
Associated Cancer: Aflatoxicosis is the disease that results from ingestion of aflatoxin. This disease can present in one of two forms. The first is an acute illness that results from exposure to large amounts of the toxin over a short period of time. Adult humans have a high tolerance for aflatoxin. Ingestion of large amounts of aflatoxin usually causes liver damage and acute illness but is rarely fatal. However, exposure to high levels of the toxin can cause death in children. The second form of aflatoxicosis is due to low level chronic exposure to aflatoxin. Chronic aflatoxin exposure has an additive effect and can lead to the development of liver cancer. Aflatoxin increases the risk of liver cancer (usually in the form of hepatocellular carcinoma or HCC) in all persons who ingest contaminated food. It can also increase the risk of lung cancer in workers who handle the grain. Infection with either the Hepatitis B or C viruses combined with exposure to aflatoxin can increase a person's risk of developing liver cancer by as much as 30 fold over a person who is exposed to aflatoxin but is not infected with hepatitis virus. Infection with the Hepatitis B virus decreases a person's ability to detoxify aflatoxin via the liver. This can partially account for the greatly increased risk of cancer development in individuals exposed to both aflatoxin and hepatitis virus.10
In its initial stages, HCC causes no noticable symptoms. It can grow for up to 3 years before causing physical symptoms.11For this reason, most HCC patients present with advanced stages of the disease, making treatment difficult. Non surgical treatments are only minimally effective. HCC patients have shown to have, at best, a 25% response rate to chemotherapy, as most HCC tumors are resistant to chemotherapy. Liver transplantation is the only current cure for HCC. Unfortunately, based on the number, size, location, and severity of the underlying disease, not all patients are candidates for a transplant.12
Infections That Cause Cancer
Although most cancer seems to arise from environmental exposures to chemicals and radiation or lifestyle choices, a large number of cases are caused by infections. As more is learned about different types of cancer, additional links with infectious agents are likely to be found.
Parasites
One of the first connections between infections and cancer was provided by Dr. Johannes Fibiger. Dr. Fibiger noticed an association between cancer in his laboratory rats and infection with a parasitic worm (nematode). He named the worm Spiroptera carcinoma. While it was later shown that the worms were not the primary cause of the cancer, the link between infection and cancer has withstood the test of time.13
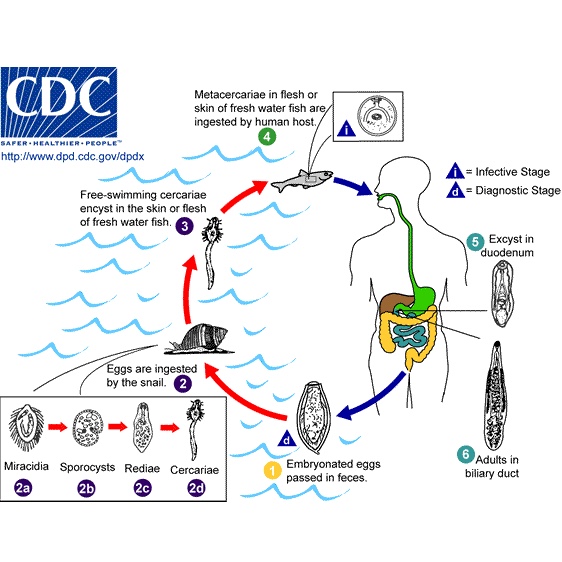
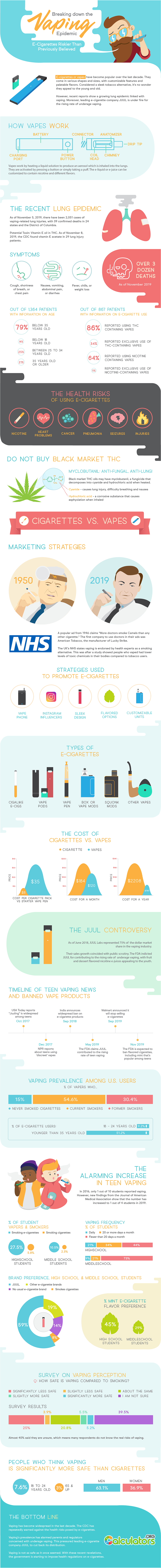
Several different kinds of worm-like parasites (trematodes) are known to cause cancer. The parasites are usually very small and have complicated life cycles, living in several different hosts at different stages in their lives. The life cycle of Clonorchis sinensis is shown above.

Schistosoma haematobium

Clonorchis sinensis

Opisthorchis viverrini
The trematodes known to cause cancer include:
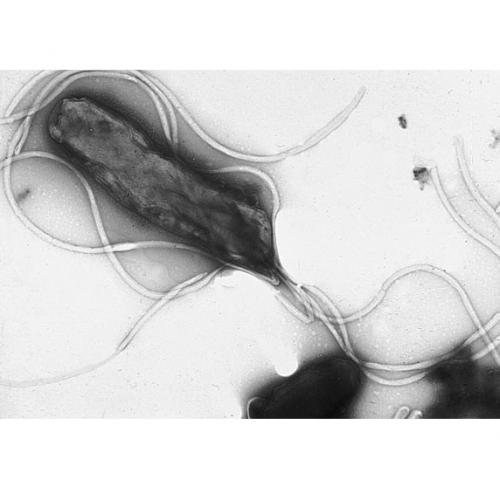
- Schistosoma haematobium causes bladder cancer. The image is a highly magified view (electron micrograph) of a schistosome.
- Clonorchis sinensis and Opisthorchis viverrini: these two 'flukes' infect the bile duct and are associated with cancer of the bile duct (cholangiocarcinoma) and liver (hepatocarcinoma).14, 15
Bacteria
Helicobacter pylori (pictured below) is a bacteria that is able to survive in the mucosa of the gastric (stomach) epithelium for a long time and is a main cause of stomach and duodenal diseases. Epidemiological studies have provided evidence that H. pylori is associated with the development of lymphoma in mucosa-associated lymphoid tissue (MALT) and gastric adenocarcinoma (stomach cancer). 16
Recent research suggests that the populations of bacteria that live in a person's instestines/colon can increase or decrease their of developing colon cancer.17, 18, 19
Viruses
Some viruses have also been associated with the initiation and promotion of tumor growth based on both epidemiological and experimental evidence. Some DNA viruses contain genes whose products can take control of cell division in the host cell. They promote the development of tumors by increasing proliferation rates and shutting down the normal systems that prevent cells from dividing. These viruses include human papillomavirus (HPV), the most significant risk factor for the development of cervical cancer. HPV also causes cancers of the head/neck, anal cancer, and urogenital cancers.20, 21 Similarly, an RNA virus, human T-cell leukemia virus type 1 (HTLV-1) leads to adult T-cell leukemia by stimulating the proliferation of infected T-cells. 22, 23, 24 Epstein-Barr virus (EBV) is another virus that increases cell proliferation. This virus also protects infected cells from death (apoptosis). EBV infects more than 90% of the world's adult population and has been implicated as a cause of Burkitt's lymphoma, nasopharyngeal carcinoma and gastric lymphoma.25, 26
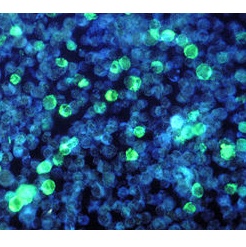
The image above shows leukemia cells infected with EBV.
Some viruses also have indirect effects on tumor development. Hepatitis B causes damage that leads to increased cell division and inflammation in the liver, potentially promoting the growth of tumors.27

Long-term infection can lead to inflammation that favors the development of cancer. The hepatitis virus (green) is an example of a virus that causes cancer this way. The immune cells (purple) cause changes in the environment that support cancer growth (red).

Type the caption here.

Type the caption here.
The human immunodeficiency virus (HIV) greatly reduces the function of the immune system and is the cause of AIDS. HIV infection may also make patients susceptible to infection by a type of human herpes virus, HHV 8, that is a risk factor for Kaposi's sarcoma28.
Learn more about viruses that cause cancer.
Obesity and Cancer
Approximately 35% of men, 40% of women, and 17% of youth (ages 2-19) in the United States are obese (based on BMI), according to articles published by the Journal of the American Medical Association in 2016 29, 30. Since 2005, there has been a slight increase in obesity in women, and the rates in men and children have remained about the same. Even in the face of large amounts of research, new drugs, and community programs to fight weight gain 31, America collectively struggles to slim down.
The evidence for the obesity-cancer connection is growing as thick as America’s waistline; more and more research shows that being obese puts people at a greater risk of developing cancer. Solid cancers associated with obesity include: colon, breast (post-menopausal), uterus, pancreas, gallbladder, liver, esophagus, kidney 32, thyroid, and ovaries. Risk is also increased for blood cell cancers, including myeloma, leukemia, and non-Hodgkin's lymphoma 33. But what does excess fat (adipose tissue) have to do with the abnormal cell behaviors seen in cancer?
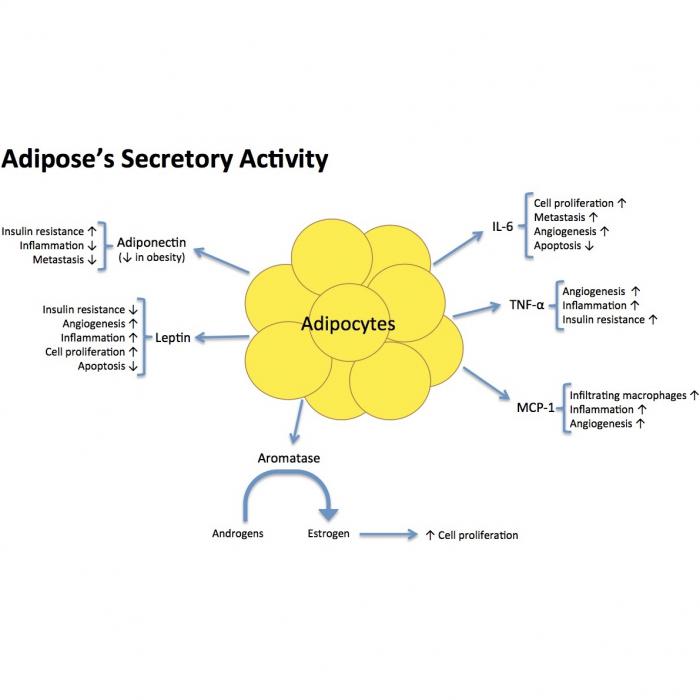
Fat as a Secretory Organ
It may help to think of fat deposits as another hormone-producing gland in the endocrine system 34(which includes the pineal gland, pancreas, ovaries, testes, hypothalamus, and adrenal glands). Fat cells actively release molecules called adipokines (“adipo-” meaning “fat” or “fatty”; “-kine” fom the Greek “kinein” meaning “to move”). Some of these adipokines can have negative effects on the rest of your body in terms of cancer development and progression 32, 35, 33, 36.
| Adipokines | Significance for Cancer |
| Leptin | Leptin’s normal job is to tell the brain when a person is full. In obese bodies, however, there is so much leptin that the brain essentially disregards the signal (“leptin resistance”). This leptin has been shown to activate pro-cell division pathways, which would lead to excessive cell proliferation 37, 34. |
| Adiponectin | Adiponectin works to counteract the effects of leptin. It can bind to growth factors to prevent them from signaling cells to divide 38. It also activates a tumor suppressor (LKB1), which inhibits metastasis 39. In addition, it can help to increase insulin sensitivity 33 and suppress expression of TNF-α and IL-6. Unfortunately, levels of adiponectin are relatively low in obese individuals. |
| Interleukin-6 (IL-6) | IL-6 is an inflammatory cytokine that is found at higher levels in obese people and during cancer development. IL-6 has been shown to activate the STAT3 pathway, which has roles in tumor cell growth and survival 40. |
|
Monocyte chemotactic protein-1 (MCP-1) |
MCP-1 is a chemokine, or a molecule that signals other cells to move. Adipocytes release MCP-1 to recruit immune cells, called macrophages, into the fat tissue. Expression of MCP-1, and the resulting macrophage infiltration and inflammation, is associated with angiogenesis and tumor progression 41. |
| Tumor necrosis factor-alpha (TNF-α) | TNF-α is an inflammatory cytokine that contributes to insulin resistance by down-regulating insulin receptors and glucose transporters 42; it can also activate the transcription factor NF-κB 32 (which leads to the expression of tumor-survival genes), and it promotes tumor cell migration and invasion 43. TNF- α is also suggested to induce adipocyte degeneration and free DNA release, which is implicated in inflammation and insulin resistance 44. See the section below on insulin resistance. |
Obesity is also associated with increased aromatase activity. Aromatase is an enzyme that produces estrogen from its building blocks (androgens). Signals from leptin, TNF-α, and IL-6 increase aromatase activity. This leads to the production of too much estrogen. Estrogen can bind to cancer cells that have the estrogen receptor, and cause them to divide 45.
Aromatase expression is also induced by prostaglandin E2 (PGE2), another inflammatory molecule elevated in obesity. PGE2 is secreted by tumor cells, macrophages, and fat cells (adipocytes) 45. When PGE2 binds to cells, it activates pathways that promote tumor growth, such as those for cell division, invasion, angiogenesis, and immunosuppression 46. PGE2 production is controlled by the enzyme cyclooxygenase-2 (COX-2), which is shown to be found at higher amounts in patients with obesity-associated breast inflammation 47.
Insulin Resistance and Cancer
When health care workers speak about the complications of obesity, they’re often referring to the complex web of conditions associated with it, including insulin resistance, high blood pressure (hypertension), increased blood sugar levels (hyperglycemia), reduced HDL cholesterol (the “good” cholesterol), elevated free fatty acids in the blood, and inflammation 48.
Insulin resistance in particular seems to be important in elevating cancer risk. When we eat, the digestive system (mouth, stomach and intestines) breaks down the meal to free up sugars in the food. The energy-packed sugars are then absorbed into the bloodstream, where they can deliver energy to the body. In response to rising blood-sugar levels, the pancreas produces insulin, which is a protein that attaches to cells and causes them to take in sugar from the bloodstream. In an individual with insulin resistance, which often occurs with obesity, the cells ‘stop listening’ to that insulin signal. Then, the cells aren’t able to take in the needed sugar, and blood sugar levels remain elevated. The pancreas tries to compensate by churning out too much insulin.
The actions of insulin and related proteins, including its receptors and insulin-like growth factor-1 (IGF-1), have been associated with increased tumor growth, particularly for colon, breast, and prostate cancer 49. The receptors for insulin can be upregulated in certain cancer cells 50, 51. When insulin binds to receptors on cancer cells, it can activate cell proliferation pathways 51 and alter the metabolism of the cells by enhancing glucose transport – the end result is that more energy is made available to the cancer cells 52.
Insulin also increases the activity of IGF-1. IGF-1 is a protein produced by the liver in response to growth hormone (GH). Normally, IGF-binding proteins 1 and 2 (IGFBP-1 and -2) bind to IGF-1 and prevent it from working. Insulin, however, can attach itself to these binding proteins, which frees up IGF-1 to do its dirty work. High IGF-1 levels have been correlated with prostate cancer, melanoma, colon cancer, and breast cancer 51. When IGF-1 binds to its receptors, it can turn on genes that control cell reproduction and cell survival 35.
A study carried out in mice and published in March 2016 suggests that obesity-induced adipocyte degeneration could lead to chronic inflammation and insulin resistance 44. When the fat cells die, their DNA is released into the surrounding tissue environment. This cell-free DNA (cfDNA) can attach to Toll-like receptor 9 (TLR9) on macrophages and cause the release of MCP-1. MCP-1 causes macrophages to infiltrate the tissue, leading to inflammation (via production of cytokines, including TNF-α) and increasing insulin resistance 53. These results were supported by studies with human blood plasma samples. Free single-strand DNA levels were higher in patients with more visceral obesity, and these patients also scored higher on HOMA-IR, an insulin resistance scale 44.
Obesity, the Microbiome, and Cancer Risk
The microbiome is the collective genes found in the hundreds of species of bacteria living inside a person. Microbiome changes have been identified as another link between obesity and cancer. The bacteria living inside the gut are usually helpful; they break down and ferment foods and hard-to-digest fibers 54, and they produce important nutrients such as biotin, vitamin K, and vitamin B12 55.
Lean and obese individuals have different mixtures of bacteria in their guts. Slimmer, healthier individuals tend to have lots of different kinds of bacteria, while obese individuals have less diversity 56. Low bacterial diversity has also been associated with insulin resistance, abnormal blood lipid content (dyslipidemia), and inflammation 57. The bacterial community seems to specialize itself depending on the diet being consumed 56. Differences in relative numbers of different kinds of microbes have been found between people with high-fat “Western” diets, plant-rich diets, or animal protein-rich diets 57.
Why does this matter? Each type of bacteria produces distinctive products (metabolites), and these can be either good or bad for one’s health. Obesity and a high-fat diet are associated with gut permeability and increases in the blood levels of bacterial lipopolysaccharides (LPS). LPS is found in the membranes of some bacteria, including E. coli 56. It is a type of toxin, and when LPS binds to its receptors (specifically, Toll-like receptor 4; TLR4)58, it can trigger an immune response by causing the release of pro-inflammatory factors such as TNF-a, interleukin 1 (IL-1), and interleukin 6 (IL-6) 56. This chronic inflammation can fuel tumorigenesis 55. LPS in the blood have also been linked to weight gain, hyperglycemia, and insulin resistance 58.
A recent study in mice (still to be validated in humans) suggests another mechanism by which the microbiome can lead to obesity and insulin resistance. Mice fed a high-fat diet had increased blood levels of acetate, which was later shown to be produced by their intestinal bacteria. This acetate would stimulate the parasympathetic nervous system, which would signal to beta-cells in the pancreas via the vagus nerve to secrete more insulin. They found that acetate also led to increased production of ghrelin, which is a “hunger hormone” that encourages a big appetite. The combination of a hearty appetite (because of too much ghrelin) and increased energy storage (because of too much insulin) is a recipe for obesity and insulin resistance 59.
To make matters worse, the types of bacteria seen in obese individuals has also been shown to be better at extracting energy or calories from food, and this can lead to further weight gain, metabolic dysregulation, and altered adipokine function 55.
Obesity and Chemotherapy
Not only does obesity increase the likelihood of developing cancer, but it can also decrease the effectiveness of some cancer treatments, including chemotherapy, targeted therapy, and anti-angiogenic therapy 60.
Bevacizumab, an anti-angiogenesis drug that prevents tumors from growing a blood supply, is used in combination with conventional chemotherapy to extend colorectal patient survival. A study published in the journal Gut suggests that visceral fat (the fat stored around the internal organs in the abdominal cavity) could be used to predict response to this bevacizumab-based therapy; more visceral fat means more tumor progression 61. The researchers think that the extra VEGF (the molecule that bevacizumab inhibits) secreted by visceral fat decreases the effectiveness of the bevacizumab.
Another retrospective study found that obese women with breast cancer developed earlier metastases and had less successful response to first-line chemo treatment with paclitaxel than non-obese women 62. Other researchers found that Chinese breast cancer patients with a higher BMI were less likely to achieve pathological complete response (defined as the absence invasive carcinoma in breast tissue and lymph nodes of in biopsy) after paclitaxel and carboplatin treatment than patients with a lower BMI 63.
Researchers found that in mouse models of pancreatic ductal carcinoma, obesity impaired the delivery and efficacy of chemotherapy drugs by decreasing vascular perfusion 64. Vascular perfusion refers to the extent of blood vessels within a tissue and the resulting delivery of nutrients (or drugs) through the bloodstream. They found that more adipocytes meant more pro-inflammatory cytokines and infiltration by tumor-associated neutrophils. This obesity-associated inflammation was coupled with desmoplasia, the growth of dense, fibrous tissue. Desmoplasia makes it easier for cancer cells to spread 65) and more difficult for blood vessels to grow properly; thus, obesity-induced desmoplasia makes it more difficult for cancer drugs to affect a tumor.
Still another study showed that the high levels of insulin often found in obese patients could activate a pathway (the PI3K/Akt pathway) that makes colon cancer cells more resistant to the chemotherapy drug, oxaliplatin 66. In fact, of current research interest is the benefit of metformin for cancer patients 60. Metformin is an anti-diabetic drug that improves insulin sensitivity, but it has also been shown to improve treatment outcomes and survival in diabetic cancer patients. In addition, metformin has been shown to reduce metastasis in animal models of pancreatic cancer. Metformin may help by inhibiting the production of inflammatory molecules and by reducing desmoplasia 60.
The large-scale clinical trials needed to determine drug dosages for obese patients have not been conducted, and there is little information available to help clinicians understand the drug dynamics of anticancer agents in obese patients 67. A 2012 report from the American Society of Clinical Oncology (ASCO) noted that up to 40% of obese cancer patients receive inadequate doses of chemotherapy 67. This could lead to an increased likelihood of remission and mortality 68. Drug doses are generally determined based on body surface area, which is calculated using a patient’s height and weight 68. This calculation can lead to some extraordinarily high-sounding doses of chemo for larger patients. Some physicians may base a patient’s dosage on their ideal body weight or an adjusted body weight, they may cap off the dose at a certain limit, or they may lower the dose due to fear of toxic side effects 69. These fears, however, are unfounded; there is no evidence for additional toxic effects from the high dosages calculated by using a patient’s actual body weight 68, 69, 67. ASCO recommends that physicians should view obese and normal-weight patients equally in terms of chemotherapy dosages with exceptions for the maximums set on the use of carboplatin, bleomycin, and vincristine 67.
Read a feature story about the connection between obesity and cancer.
Chronic Inflammation and Cancer Development
Chronic inflammation has been seen, both experimentally and epidemiologically, to be an important factor in tumor development. Chronic inflammation can be caused by viral or bacterial infections, autoimmune diseases and inflammatory conditions of unknown origins. It has been shown that mutation of key inflammatory control genes is associated with a higher risk of cancer progression, and markers of inflammation correlate with a worse prognosis for cancer patients. Inflammation seems to lead to the development of cancer because of the activities of leukocytes, including the production of proteins that alter the behavior of target cells (cytokines and chemokines), stimulation of blood vessel growth (angiogenesis) and tissue remodeling. Immune cells also produce oxygen radicals that can cause mutations in DNA.
Inflammation can both induce carcinogenesis and lead to progression and metastasis. The activation of a specific transcription factor,NF-kB, by pro-inflammatory cytokines has been shown to produce a more aggressive cancer phenotype including resistance to normal growth control mechanisms, angiogenetic capability and metastasis. Tumor associated macrophages (TAM), are also associated with the inflammatory pathway, have been observed to produce pro-angiogenic factors and recruit blood vessels early in tumor development. TAM also increase the growth rate of tumor cells and cause the dissolution of the connective tissue matrix surrounding the tumor, enabling tumor growth and spread. 70
There are several cancer types associated with chronic inflammatory conditions, including; colon cancer and inflammatory bowel disease, liver cancer and hepatitis C, bladder or colon cancer and schistosomiasis (a chronic parasitic infection) and stomach cancer and H. pylori infection. 71
Detecting Carcinogens: The Ames Test
Bacteria have proven to be good models for determining the mutagenic potential of compounds. Bruce Ames, a biochemist, developed an assay to identify potential mutagens. The Ames test works 'backwards' from what one might expect. The test starts with mutant bacteria and looks for chemicals that can change them back into normal (wild type) bacteria.
In the Ames test, a potential mutagen is placed on a paper disc in the center of a petri dish on which only bacterial cells that mutate are able to grow. The mutagenic potential of the compound in question is determined by the amount of bacterial growth seen. Information obtained in this way was shown to be comparable to results from tests in rodents. The Ames test has been used since 1973 and is still a standard test for detecting potential mutagens and carcinogens.72
Researchers have also manipulated mouse cells to make them potential targets for carcinogens and have transferred genes from cancerous cells into healthy cells and animals. All of the research has led to the conclusion that mutations in key genes can lead to changes that result in cancer. 73, 74
List of Carcinogens and the Cancers They Cause
|
Agent |
Cancer Type |
|
Mouth, Pharynx, Larynx, Espohagus |
|
|
Respiratory-tract, Pleural and Peritoneal Mesothelioma |
|
|
Endometrial, Ovarian, Breast |
|
|
Endometrial |
|
|
Childhood Cancer |
|
|
Childhood Cancer |
|
|
Liver |
|
|
Scrotal |
|
|
Lung, Nasal |
|
|
Nasal |
|
|
Respiratory-tract, Lung |
|
|
Bladder |
|
|
B-cell Lymphoma, Nasal, Pharyngeal, Stomach |
|
|
Kaposi's Sarcoma |
|
|
Brain |
|
|
Liver |
Tobacco
Tobacco is an herbaceous plant belonging to the Solanaceae family. The primary source of commercial tobacco is cultivated and harvested Nicotiana tabacum 78, 79. Tobacco leaves contain nicotine, the chemical responsible for tobacco's addictive effects. To get these effects, the leaves can be chewed, smoked, or sniffed. Nicotine's effects on the body include decreased appetite, elevated mood and feeling of well-being, increased heart rate and blood pressure, and stimulated memory and alertness. These effects don't last long and may be replaced by symptoms of nicotine withdrawal within 2-3 hours after the last tobacco use. Symptoms of nicotine withdrawal include intense nicotine cravings, anxiety, depression, restlessness, headaches, increased appetite, and concentration problems 80. The intensity of nicotine's effects as well as nicotine withdrawal symptoms depends on the level of nicotine present in the body. In 1993 in the U.S, Brown & Williamson Tobacco Corporation specially bred a type of tobacco known as Y-1 by using genetically altered tobacco seeds. The Y-1 breed of tobacco was reported to have had the highest known nicotine yield in tobacco at that time, at 6.2% compared to the 2.5-3% found in typical flue-cured tobacco. Y-1 tobacco was used in five brands of American cigarettes, but its usage was discontinued when the Food and Drug Administration (FDA) became concerned with nicotine-level manipulation 81.

Nicotiana tabacum
Chemical structure of nicotine

Tobacco field
Tobacco Timeline
- 1st century BC – Earliest archaeological evidence indicates smoking in Mayan civilization 82
- 1612 – Chinese ban growing and smoking tobacco 82
- 1723 – Berlin bans smoking 82
- 1761 – Englishman John Hill claims that using too much snuff could cause nose cancer 82
- 1910 – U.S. tobacco taxes amounts to approximately $13 million this year 82
- 1912 – Isaac Adler raises concern that cigarettes might cause lung cancer 82
- 1921 – Smoking is illegal in 14 American states though bans are removed within the decade 82
- 1930s – Tobacco provides approximately 8% of Germany's entire national tax income 82
- 1964 – Surgeon General's report on cigarettes and tobacco (42) 1970s – U.S. tobacco taxes amounts to approximately $5 billion 82
- 1971 – Radio and television advertising for cigarettes is banned 83
- 1998 – Attorney generals of 46 U.S. states and major tobacco corporations agree upon the Tobacco Master Settlement Agreement 84
- 2001 – Tobacco provides approximately 10% of China's entire national tax income 82
- 2003 – Hon Lik of Beijing, China, invents the electronic cigarette (e-cigarette) 85
- 2006 – E-cigarettes are introduced to Europe and the U.S. 85
- 2014 – CVS, a major U.S. pharmacy chain, announces its intention to stop selling tobacco products by October 1, 2014 86
Common Usages
Tobacco leaves can be smoked or used in a smokeless form.
Smoking Tobacco
Overview
Smoking tobacco refers to tobacco that is heated and smoked. Some common examples of smoking tobacco include cigarettes, cigars, and hookahs. It is important to note that while e-cigarettes do not contain tobacco and are not burned during use, their rise in popularity as "smoking" devices has led the FDA to begin regulating e-cigarettes 87. A section on e-cigarettes is included below.
Sir Walter Raleigh brand smoking tobacco
Cigarettes
Each cigarette typically contains less than 1 gram of tobacco. Cigarettes are made of hundreds of chemicals that react in the presence of heat to produce thousands of chemicals. Many of the chemicals that have been identified as cancer-causing agents (carcinogens) can be found in the sticky, partially burned residue known as "tar". Some of the remaining thousands of chemicals have been identified as toxic substances that may damage a person's health 80. Some examples of the chemicals found in tobacco smoke are arsenic (also found in rat poison), butane (also found in lighter fluid), cadmium (also found in battery acid), carbon monoxide (also found in car exhaust fumes), nicotine (also used as insecticide), and toluene (also found in paints) 88. Smoking tobacco produces several powerful cancer-causing chemicals, including nitrosamines and benzo(a)pyrene.

Lit cigarette
Cigars
Each cigar can contain between 1-20 grams of tobacco, depending on the size of the cigar. Cigar smoke contains higher levels of toxins and carcinogens than cigarette smoke due to the type of tobacco and wrapping used. The tobaccos used in cigars are fermented, producing higher levels of carcinogenic nitrosamines, which are released into the air when a cigar is smoked. Furthermore, cigar wrappers are less porous than cigarette wrappers, so there is less complete burning of cigar tobacco than of cigarette tobacco, resulting in higher levels of toxins in cigar smoke. Although most cigar smokers do not deeply inhale cigar smoke while smoking, they are still exposed to the carcinogenic substances 89.

Nicaraguan cigar

Cigar makers
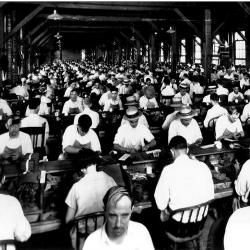
Ybor City cigar factory workers
Hookahs
Hookahs are water pipes used to smoke flavored tobacco. Hookah smoking has similar health risks as cigarette smoking, and hookah smoke is comparable in toxicity to cigarette smoke. Depending on the length of a hookah smoking session, hookah smoking may be more detrimental to smokers' health because hookah smokers may end up inhaling more toxic chemicals than if they were to quickly smoke a cigarette. On average, approximately 90,000mL (about the volume of 24 one-gallon milk jugs) of smoke is inhaled during a 1-hour hookah smoking session, while 500-600mL (about the volume of a 1-pint milk carton) of smoke is inhaled when smoking a cigarette 90, 91, 92. In a 2018 study of users aged 18-34, hookah use for just 30 minutes was shown to result in stiffening of blood vessels, increased heart rate, and increased blood pressure. Increased arterial stiffness is linked to heart disease.93 In addition, if the hookah mouthpiece is shared among several people, there is also the possibility of transmitting infectious diseases, such as herpes, hepatitis, tuberculosis, and others 94.

Hookah
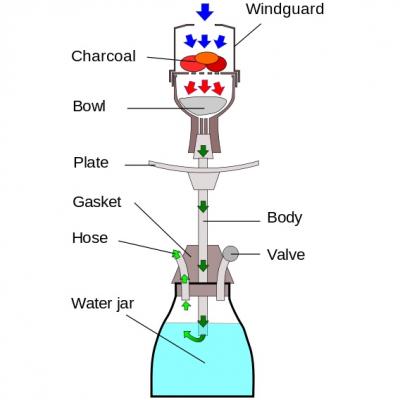
Parts of a hookah
E-cigarettes
E-cigarettes are battery-powered devices that are typically designed to look like common objects, such as cigarettes, cigars, pens, pipes, and USB drives. These devices do not contain tobacco. Instead, they deliver nicotine in aerosol form for users to inhale 95. The FDA has found levels of carcinogenic nitrosamines and other toxic substances (ex: some chemicals also found in anti-freeze) in certain e-cigarette liquids. More research is needed to determine exactly what e-cigarettes contain, how they are used, and their effects on users. According to a study funded by the National Institutes of Health, researchers observed that rising high school students who had previously used e-cigarettes, but not combustible tobacco products, were more likely to start using combustible tobacco products over the following 12 months, compared to rising high school students who had never used e-cigarettes or combustible tobacco products 96. As of May 2014, the FDA has not yet approved e-cigarettes as devices that help people quit smoking 97. The FDA began regulating e-cigarettes in 201687. The regulations would involve minimum age restrictions, inclusion of health warning labels, and more. In June of 2017, a team of researchers from the University of Connecticut found that e-cigarettes may be just as dangerous, in some ways, as unfiltered cigarettes. Even e-cigarettes without any nicotine caused amounts of DNA damage that were comparable to filtered cigarettes. DNA damage leads to mutations, permanent changes that can trigger the development of cancer.98 Several different studies have shown that using e-cigarettes can impact cardiovascular health, including altering heart rates and increasing vascular stiffness. 99, 100, 101

Electronic cigarette
Smokeless Tobacco
Overview
Smokeless tobacco refers to tobacco that is used in ways that do not involve burning the tobacco. Examples of smokeless tobacco include chewing tobacco and snuff. Smokeless tobacco contains over 30 known carcinogens. Examples include the nitrosamines, NNK (4-methylnitrosamino-1-3-pyridyl-1-butanone), and NNN (NL';-nitrosonornicotine). There are approximately 1-5 μg of NNK and NNN present in every gram of smokeless tobacco. Smokeless tobacco users are exposed to 100-1000 times more carcinogenic nitrosamines than nonusers. The carcinogens listed above, along with their metabolites (metabolites are additional chemicals produced when the body processes something that has been taken in), can be detected in saliva and urine samples. Studies suggest that NNK and NNN that have been processed in the body may cause DNA changes in mouth tissues, which can lead to permanent DNA damage. DNA damage to important genes, such as RAS and P53, can result in cancer. Additionally, the metabolism of carcinogens produces reactive chemicals that could lead to chronic inflammation and irritation in the body 102.
Chewing tobacco
Chewing tobacco are loose tobacco leaves that are chewed and spat out. Chewing releases the nicotine present in tobacco, and the nicotine is absorbed through mouth tissues 103. Chewing tobacco was the most prevalent form of tobacco in the U.S. prior to the cigarette industry expansion in 1918. 102

Chewing tobacco
Snuff
Snuff is found in 2 forms: dry snuff and moist snuff. Dry snuff is a form of powdered tobacco that is inhaled through the nose, while moist snuff, also known as dipping tobacco, is marketed as a discreet way of using tobacco. Moist snuff is placed in the mouth so that the nicotine is absorbed through the mouth tissues. 103 Snuff is the most prevalent form of smokeless tobacco in some countries, including Sweden. 102

Impacts on Health
Overview
Smoking and smokeless tobacco usage not only impacts the user but can also harm those exposed to tobacco smoke. Studies have shown that tobacco is also detrimental to the health of the children and grandchildren of tobacco users. In 1964, the U.S. Surgeon General's office released a landmark report on the health effects of tobacco usage. On the 50th anniversary The Surgeon General released an update on the progress made in reducing tobacco deaths and illness. 104. We now know that all forms of tobacco are harmful to the user and, frequently, to those nearby. Tobacco's negative impact can even extend to unborn future offspring of users.
Smoking Tobacco
Firsthand Exposure
- What is it?
- Firsthand exposure refers to the tobacco smoker's exposure to tobacco smoke and its many toxins.
- Prevalence
- In 2012, approximately 18.1% of U.S. adults (at least 18 years old) were cigarette smokers. Among the smokers, 78.4% of them smoked every day 105.
- Health problems
- There are many health-related issues associated with smoking tobacco, including cancer, brain damage, heart disease, stroke, lung disease, and wrinkles.
- Cancer
- Smoking tobacco is linked to many types of cancers, including cancer of the mouth, nose, throat, larynx, esophagus, lung, stomach, liver, pancreas, kidney, blood and bone marrow, colon, and intestine 106.
- Heart Disease and Stroke
- Cigarette smoking causes coronary heart disease, the leading cause of deaths in the U.S. It has been found that cigarette smokers are 2-4 times more likely to develop coronary heart disease than nonsmokers and are twice as likely to have a stroke 107.
- Brain damage
- Present in all forms of tobacco, the carcinogen NNK has been found to cause brain damage by causing immune cells to attack healthy brain cells 102.
- Wrinkles
- Although wrinkles are not a serious health concern, studies have found that smoking is linked to the breakdown of elastin fibers, which are the protein bundles responsible for the skin's ability to stretch and relax. Loss of elastin fibers results in skin wrinkles 108.
- Cancer
- There are many health-related issues associated with smoking tobacco, including cancer, brain damage, heart disease, stroke, lung disease, and wrinkles.
- Lung Disease
- Chronic obstructive pulmonary disease (COPD) is a broad term that covers lung diseases including emphysema and chronic bronchitis. COPD refers to serious lung diseases. Patients have less airflow through their airways, making it harder for them to breathe. This condition can occur when the tiny air sacs in the lungs lose their ability to stretch and shrink, when the walls separating the air sacs become damaged or inflamed, or when the airways are obstructed by abnormal amounts of mucus 106, 109, 110, 111. Smoking is responsible for 9 out of 10 COPD-related deaths 109. Smoking has also been found to trigger asthma attacks 112.
- Loss of Y Chromosome
- Recent studies suggest that male smokers are at a significantly greater risk of losing their Y chromosome. Specifically, male smokers were found to be up to 4 times more likely to have blood cells that have lost the Y chromosome 113. The Y chromosome is the chromosome that contains sex-determining genes. Previous studies have suggested that loss of Y chromosome may be associated with a shorter lifespan and a greater risk for developing cancer 114.
Secondhand Exposure
- What is it?
- Secondhand exposure to smoke it the involuntary or passive exposure of nonsmokers to tobacco smoke. The two types of tobacco smoke relevant to smoke exposure are called mainstream smoke and side stream smoke. Mainstream smoke refers to the smoke that is exhaled by a smoker, while side stream smoke refers to the smoke that comes from the lit end of a cigarette, cigar, pipe, and other tobacco-smoking devices. While all secondhand smoke exposure is regarded as harmfull, side stream smoke is considered to be more toxic than mainstream smoke because side stream smoke contains higher concentrations of carcinogens 115.
- >When a person is exposed to secondhand smoke, the nicotine in the smoke is changed by the body (metabolized) into cotinine, a nicotine byproduct which can be detected in saliva, urine, and blood samples 116, 117.
- Prevalence
- Although secondhand smoke exposure (measured by cotinine levels) has decreased among U.S. nonsmokers and among all racial and ethnic groups, it still remains higher among non-Hispanic black Americans than among non-Hispanic white Americans and Mexican Americans. The percentage of nonsmokers who had measurable levels of cotinine in their system decreased from 87.9% (1988-1991) to 40.1% (2007-2008). It was estimated that approximately 88 million U.S. nonsmokers were exposed to secondhand smoke in 2007-2008 118, 117.
- Health problems
- There are many health-related issues associated with secondhand smoke, including cancer, pregnancy problems, heart disease, stroke, and lung problems.
- Cancer
- Birth and Pregnancy
- Secondhand smoke exposure has been found to increase the risk of a miscarriage, stillborn birth, and other pregnancy-related problems 115.
- Heart Disease and Stroke
- Lung Disease
- Secondhand smoke exposure is responsible for approximately 7,500 to 15,000 annual hospitalizations of U.S. children aged 18 months and younger and is responsible for approximately 150,000 to 300,000 annual cases of bronchitis and pneumonia in U.S. children aged 18 months and younger 116, 117. Secondhand smoke has also been found to trigger asthma attacks 112
- There are many health-related issues associated with secondhand smoke, including cancer, pregnancy problems, heart disease, stroke, and lung problems.
- Preventative Measures
- Ways to avoid secondhand smoke exposure and to protect from its damaging effects include, but are not limited to, the following: not being exposed to secondhand smoke, preventing indoor smoking, filtering the air, and ventilating buildings 115.

Thirdhand Exposure
- What is it?
- Thirdhand exposure to smoke refers to the involuntary or passive absorption, through the skin or ingestion through the mouth, of carcinogenic tobacco residues that may be found on surfaces or mixed with the dust in the air. Thirdhand exposure is most prevalent among babies and children who are more inclined to touch surfaces and subsequently lick their hands. The health effects of thirdhand exposure to smoke are still under study 115.
Transgenerational effects
- What is it?
- Tobacco exposure not only affects the health of the smoker but can also affect the health of the smoker's children, grandchildren, and so on. The toxins and carcinogens present in tobacco smoke can cause unfavorable genetic and epigenetic* changes to the smoker's DNA as well as to the smoker's descendants' DNA, which could lead to genomic instability and damaged DNA repair systems. The mechanisms of how this works is still under study 119.
*Epigenetic changes refer to slight chemical modifications that control the "on" or "off" status of a gene. These changes are not the same as mutations, which refer to alterations of the 'letters' of the DNA sequence itself. An epigenetic change would be like changing the letter 'a' into the letter 'A'. They are similar, but not the same. A mutation would be like changing the letter 'a&' to the letter 'b'. They are very different.
- Recent studies of epigenetic changes suggest that the amount of methylation (a form of epigenetic change) of the F2RL3 gene may serve as a measure of a person's lifetime exposure to firsthand tobacco smoke. This means that F2RL3 methylation has the potential to help determine a person's risk for developing smoking-related cardiovascular diseases 120. Other studies have found that the toxins in tobacco smoke can lead to epigenetic changes within reproductive cells (sperm/egg). Specifically, changes in the expression of important microRNAs (miRNAs) in human spermatozoa have been found. Researchers believe that these epigenetic changes are heritable and may affect sperm health and the development of the embryo 121. A study using rats suggests that maternal smoking during pregnancy could result in nicotine-induced asthma in children, grandchildren, and subsequent generations 122, 123.
Structure of DNA
E-cigarette Poisoning
- What is it?
- E-ciagrette poisoning happens when e-cigarette liquid containing nicotine is ingested, inhaled, or absorbed through the skin or eyes. This can lead to vomiting, nausea, eye irritation, heart problems, and even death. According to a CDC study, there has been an increase in the number of calls received by U.S. poison centers regarding e-cigarette liquids (1 call per month in 2010 to 215 calls per month in 2014). There was no similar increase in the number of calls received regarding conventional cigarettes. Furthermore, approximately 51% of calls regarding e-cigarette poisoning involved children under the age of 5, and approximately 42% of calls regarding e-cigarette poisoning involved people aged 20 and older 124. Another recent source reports that in 2013, 1,351 calls were received by poison control centers in the U.S> regarding e-cigarette liquids, three times more than the number of calls received in 2012. Furthermore, 365 of those 1,351 calls were referred to hospitals, also three times more than in 2012. Currently, e-cigarette liquids are sold online to the general public by the liter (about one quart) at nicotine concentrations as high as 10% 125. According to a study conducted at Washington University School of Medicine in St. Louis, many parents fail to safely store e-cigarette liquids and few parents were aware of the risks associated with unsafe e-liquid storage. 36% of the e-cigarette users surveyed did not lock up e-liquid bottles after use and did not use childproof caps. Also among those surveyed, 3% reported instances where their child attempted to consume the e-liquid 126. On January 2, 2020 the FDA announced a ban on flavored e-cigarettes that appeal to children. Some flavors are not covered by the ban.127.
E-cigarette Fires and Explosions
- While fires and explosions caused by e-cigarettes are rare, they can cause serious injuries and burns when they do occur. Between 2009 and 2014 in the United States, 25 incidents involving e-cigarette explosion and fire were reported. These 25 incidents were associated with 9 injuries and 0 deaths. 128 Most e-cigarette explosions result from the spontaneous ignition and explosion of e-cigarette batteries during e-cigarette use or during e-cigarette battery charging. These explosions can cause internal and external burns to the user's face, neck, throat, lungs, and more. 129, 130 E-cigarette batteries have also spontaneously exploded when it is not in use or charging. 131
Smokeless tobacco
Firsthand exposure
- What is it?
- Firsthand exposure refers to the user's exposure to the dangerous chemicals found in smokeless tobacco.
- Prevalence
- It was estimated that in 2012, about 9 million people aged 12 and older living in the U.S. used smokeless tobacco. Smokeless tobacco usage is higher among younger age groups. According to CDC's 2012 National Youth Tobacco Survey, smokeless tobacco usage is higher among high school-aged people than among young adults between the ages of 18 and 25 103.
- Health problems
- There are many health-related issues associated with using smokeless tobacco, some of which include cancer, heart disease, mouth sores (leukoplakia), and dental problems.
- Cancer
- Smokeless tobacco usage is linked to various types of cancers, such as those of the mouth, tongue, cheek, gum, throat, esophagus, stomach, and pancreas 103.
- Heart disease
- Although more studies are needed to identify the role of smokeless tobacco in heart diseases, current data suggests that smokeless tobacco users are more likely to have heart disease, high blood pressure (hypertension), and heart failure than those who do not use smokeless tobacco 103.
- Dental
- Smokeless tobacco usage is linked to cavities and tooth decay 103.
- Leukoplakia
- Leukoplakia refers to white mouth lesions that can become cancerous. These oral soft tissue abnormalities are most commonly found in smokeless tobacco users, at the site where smokeless tobacco is placed 102.
- Cancer
- There are many health-related issues associated with using smokeless tobacco, some of which include cancer, heart disease, mouth sores (leukoplakia), and dental problems.

Additional statistics
Deaths
- Smoking tobacco is responsible for approximately 1 in every 5 deaths (includes exposure to firsthand and secondhand smoke), which translates to more than 480,000 deaths in the U.S. each year. Men account for approximately 279,000 of those annual deaths, while women account for approximately 202,000 of those annual deaths 132, 133, 134. As a comparison, there are 525,949 minutes per year, so that works out to nearly one death from smoking every minute.
- From 2005-2009, it was estimated that approximately 42,000 annual deaths among nonsmokers were due to secondhand smoke exposure. Among those 42,000 annual deaths, approximately 7,300 deaths were due to lung cancer, while approximately 34,000 annual deaths were due to heart disease 117. It is estimated that at least 30% of all cancer deaths are due to tobacco use 135. It was also estimated that, since 1964, approximately 2.5 million nonsmokers have died due to secondhand smoke exposure 117.
Life expectancy
- According to the World Health Organization, 1 in 2 lifetime smokers will die of a disease associated with tobacco use 136. According to the Centers for Disease Control & Prevention (CDC), U.S. nonsmokers live at least 10 years longer than U.S. cigarette smokers 132, 133, 137.
Preventable deaths
- An estimated 1 out of every 3 cancer deaths in the U.S. could be prevented if no one smoked tobacco. A smoker's risk for getting mouth, throat, esophageal, and bladder cancer decreases by half within 5 years of quitting smoking, and a smoker's risk of dying from lung cancer decreases by half within 10 years of quitting smoking 138.
Economy
Economic costs
- According to the 2014 Surgeon General's Report, from 2009 to 2012, U.S. lost an estimated $289-332.5 billion each year due to smoking-related economic costs 133.
- Approximately $132.5-175.9 billion of the $289-332.5 billion lost was due to direct medical care for adults between the ages of 35 and 79, approximately $151 billion of the $289-332.5 billion was productivity loss due to premature deaths of adult smokers aged 20 and older (using 2005 to 2009 data), and $5.7 billion of the $289-332.5 billion was productivity loss due to secondhand smoke exposure (using 2006 data) 133.
- Of the $5.7 billion productivity loss due to deaths from secondhand smoke exposure, approximately $4.6 billion was due to deaths from coronary heart disease, while $1.1 billion was due to deaths from lung cancer 139, 133.
- It is estimated that the health and productivity costs for every pack sold in the U.S. is $18.20 per pack 140.
Tax income
- It is estimated that in 2014 in the U.S., states will generate approximately $25 billion in tobacco revenue from tobacco taxes and the 1998 Tobacco Master Settlement Agreement.
- Only 1.9% of that revenue will be spent towards smoking prevention and cessation programs. As of April 2014, there were no states in the U.S. that met CDC's "recommended" level for amount of money allocated towards tobacco control programs 141, 142, 143, 133.
Economies of different tobacco products
- Cigarettes
Sales
The number of cigarettes sold or given away by manufacturers decreased from 2010 to 2011 by 2.9% 144. Still, in 2011, more than 293 billion cigarettes were sold in the U.S. Of those, 135.1 billion were sold by Philip Morris USA (Brand examples: Marlboro, Basic, Virginia Slims), 72.9 billion were sold by Reynolds American Inc. (Brand examples: Camel, Doral, Winston, Kool), 40 billion were sold by Lorillard (Brand examples: Newport, Maverick, Kent), and the remaining 45 billion were sold by several other companies 145.
>Advertising
>The amount of money spent on cigarette advertisements and promotions increased from $8.046 billion (2010) to $8.366 billion (2011). Of the $8.366 billion, $7.0 billion was spent on cigarette price discounts 144.
Leaderboard
Cigarette consumption in 2009 146
1. China (most cigarettes consumed)
2. Russia
3. United States
4. Indonesia
5. Japan
Cigarette production in 2010 147
1. China (produced 41% of world's cigarettes)
2. Russia (7%)
3. United States (6%)
4. Germany (4%)
5. Indonesia (3%)
Cigarette export in 2010 147
1. Germany (exported 181.11 billion cigarettes)
2. Netherlands (115.35 billion)
3. Poland (89.49 billion)
4. United States (60.45 billion)
5. Indonesia (57.40 billion)
- Cigars
Sales
In 2011, approximately 13.7 billion cigars were sold in the U.S. Of those 13.7 billion cigars sold, 2.9 billion were sold by Swisher International (Brand examples: Swisher Sweets, Universal), 2.5 billion were sold by Cheyenne International, LLC (Brand examples: Cheyenne, Derringer, Bodyshot), 1.59 billion were sold by Altadis USA (Brand examples: Dutch Masters, Phillies), 0.55 billion were sold by Prime Time International, and the remaining 7.11 billion were sold by several other companies 145.
-
E-cigarettes
Sales and Revenue
Since they first appeared in the consumer market in 2005, e-cigarettes have rapidly grown in popularity. From 2009 to 2012, U.S. e-cigarette sales increased at an annual rate of 115%. Estimates predict that U.S. e-cigarette sales will reach $2 billion in 2014 and global e-cigarette sales will reach $10 billion by 2017 148, 149.
Over 95% of the world's e-cigarettes are produced in Shenzhen, China. Speculators believe that the e-cigarette market could see a rapid expansion as more public smoking bans are instituted in China 148.
Advertising
Exposure to e-cigarette TV ads among adolescents aged 12 to 17 increased by 256% from 2011 to 2013 in the U.S. Exposure to e-cigarette TV ads among young adults aged 18 to 24 increased by 321% from 2011 to 2013 in the U.S. 150.
As of January 2014, researchers at the University of California, San Diego, have found over 460 different English-language e-cigarette websites, each marketing its own brand of e-cigarettes. On those English-language e-cigarette websites, researchers discovered almost 7,800 different e-cigarette flavors and estimated that around 10 new e-cigarette brands and 240 new e-cigarette flavors appeared online each month during their study. The researchers also found that approximately 10% of e-cigarette companies had falsely claimed that e-cigarette products could help smokers quit smoking 149.
-
Smokeless Tobacco
Sales and Revenue
The amount of smokeless tobacco sold by manufacturers to retailers and wholesalers increased from 122.6 million pounds (2010) to 124.6 million pounds (2011). Of those 124.6 million pounds sold in 2011, 56 million pounds were sold by U.S. Smokeless Tobacco Company (Brand examples: Copenhagen, Skoal), 35.3 million pounds were sold by American Snuff (Brand examples: Grizzly, Kodiak), 20.9 million pounds were sold by Swedish Match (Brand examples: Timber Wolf, Red Man), and the remaining 12.4 million pounds were sold by several other companies 145, 151.
The following monetary values are presented in nominal values and have not been adjusted for inflation. The revenue generated by manufacturers rose from $2.78 billion in 2010 to $2.94 billion in 2011 152.
Advertising
The amount of money spent on smokeless tobacco advertisements and promotions increased from $444.2 million (2010) to $451.7 million (2011) 152.
Regulations
The following represents a selected list of U.S. laws and regulations that fall under the jurisdiction of certain U.S. government agencies, with the purpose of governing tobacco sales, advertisements, and usages. Additional tobacco laws and regulations can be found here.
Alcohol and Tobacco Tax and Trade Bureau (TTB)
Relating to tobacco regulation, TTB is responsible for enforcing laws that regulate business engagements in tobacco manufacturing and importing, such as those that deal with federal excise taxes on tobacco products, cigarette papers and tubes, and more. TTB is not responsible for enforcing laws that deal with the age of tobacco buyers, sellers, and users; it is the responsibility of each state’s government to enforce those laws and regulations 153
Bureau of Alcohol, Tobacco, Firearms and Explosives (ATF)
Prevent All Cigarette Trafficking Act of 2009 (PACT Act) is a an act signed by President Barack Obama on March 31, 2010 designed to prevent tobacco smuggling and to enforce tobacco sales and tax laws.
Comprehensive PACT Act

Federal Trade Commission
Federal Cigarette Labeling and Advertising Act of 1965 is an act passed by Congress that governs cigarette labeling and advertising. This act requires the Federal Trade Commission (FTC) to annually report to Congress on the current status of cigarette labeling and advertising practices. This act also requires that health-warning labels be present on all cigarette packages 154
Food and Drug Administration (FDA)
Family Smoking Prevention and Tobacco Control Act (Tobacco Control Act) is a tobacco regulation law signed on June 22, 2009 designed to protect public health. Under this law, the FDA has the power to regulate the manufacture, distribution, and marketing of tobacco products 155
Overview of the Tobacco Control Act
Comprehensive Tobacco Control Act
Learn about how the FDA regulates tobacco products
In 2022, the FDA published plans for future regulations on tobacco. The proposal would set a maximum for the amount of nicotine in cigarettes and other burnable tobacco products. The goal is to reduce the addictiveness of these tobacco products.156, 157
U.S. Office of Attorney Generals
In 1998, concluding the largest financial recovery civil lawsuit in U.S. history, the attorney generals of 46 states reached a settlement known as the Tobacco Master Settlement Agreement of 1998 (MSA) with four major U.S. cigarette companies (Philip Morris, R.J. Reynolds, Brown & Williamson, and Lorillard). In this settlement, tobacco companies agreed to pay approximately $206 billion through the year 2025 to help compensate for the health care costs and damages brought forth by tobacco usage in the U.S. 158. In exchange, each of the 46 states agreed to withdraw their claims that tobacco companies were in violation of state antitrust and consumer protection laws. The MSA also imposed new limits to govern tobacco advertising and marketing and allocated money towards anti-tobacco education, with the intent of better protecting minors 158, 159
Comprehensive Master Settlement Agreement
Cessation Resources
Centers for Disease Control and Prevention (CDC)
Tips From Former Smokers campaign
Additional quitting smoking resources
American Cancer Society
Comprehensive guide to quitting smoking
Comprehensive guide to quitting smokeless tobacco
Help for cravings and tough situations
General tips for family and friends of smokers who are trying to quit
Additional quitting smoking and quitting smokeless tobacco resources
U.S. Department of Health and Human Services
Starting and continuing on a smoke-free journey
U.S. Food and Drug Administration
FDA-approved tobacco cessation products
Non-profit Organizations
The graphic below, from Calculators.org, presents a detailed infographic about tobacco use. Visit their site to view more about tobacco usage and e-cigarettes.
Vaping Infographic provided by Calculators.org
Alcohol
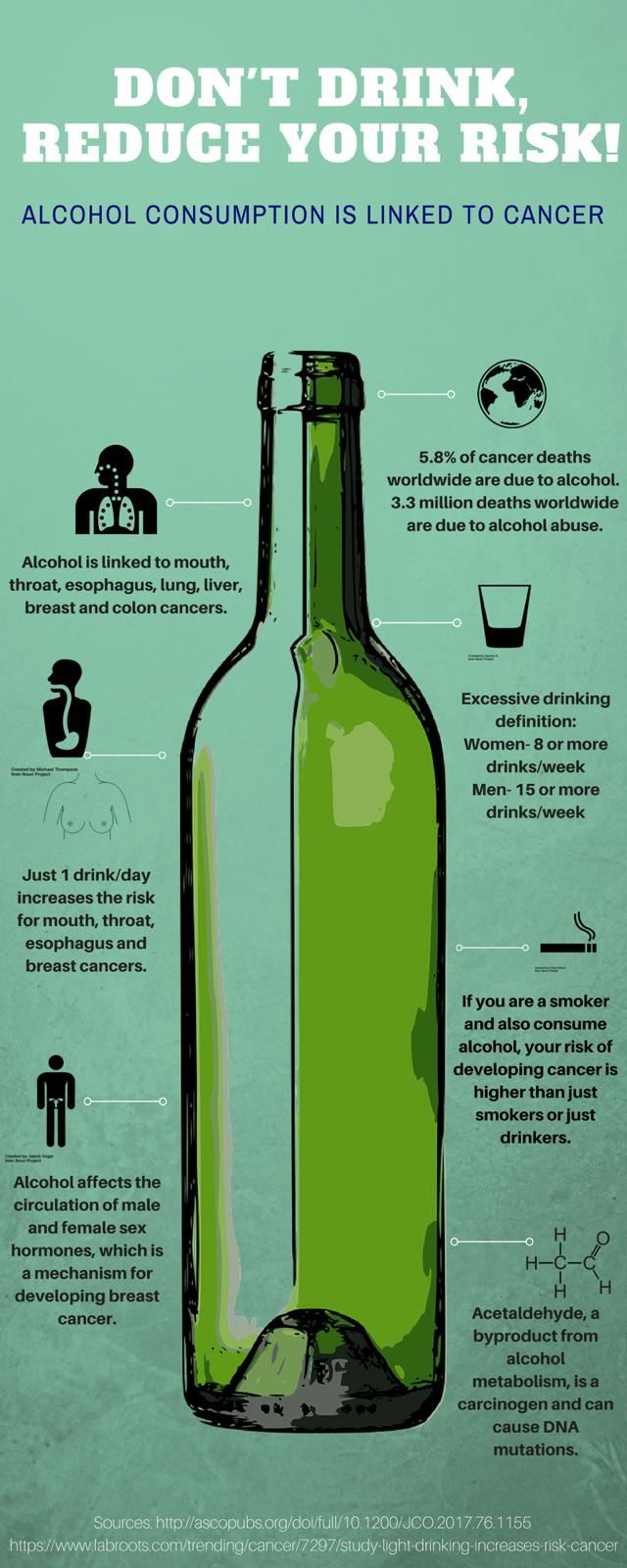
Alcohol Consumption and its Link to Cancer:160
Children and young adults who drink alcohol have a higher risk of misusing alcohol when they become adults. The majority of adults at high risk for alcohol abuse started drinking before the age of 21. Drinking alcohol moderately or heavily over long periods of time are risk factors for cancer.
The link between alcohol consumption and risk of developing cancer is a dose-response relationship: if developing a specific type of cancer is associated with drinking alcohol, then the more one consumes alcohol, the higher the risk for cancer. Alcohol consumption is linked to cancers of the mouth, throat, esophagus (the tube running down from your throat to your stomach), liver, breast, colon and rectum. This link has been observed across different types of alcoholic beverages- wine, beer, spirits and hard liquor.
Light drinkers are at risk for developing mouth and esophageal cancers, with the highest risk for esophageal cancer. Moderate drinkers are at risk for mouth, throat and esophageal cancers, and just like light drinkers, their highest risk is for esophageal cancer. Heavy drinkers are at risk for the same cancers as moderate drinkers, but their greatest risk is for mouth cancer.
How Does Alcohol Cause Cancer?
Alcohol on its own isn’t a carcinogen (a substance known to cause cancer). When we consume alcohol, it is broken down and converted into a form that can be eliminated from the body. This form is a chemical called acetaldehyde, which is a carcinogen that can stick to our DNA and cause harmful changes (mutations) in our genes. In animal experiments, mice and rats which drank water with added alcohol or acetaldehyde developed tumors. Consuming alcohol also cause inflammation.
In cells, alcohol is broken down through a series of steps. One protein involved in this process is called aldehyde dehydrogenase-2 (ALDH2). As stated before, alcohol is converted to acetaldehyde. ALDH2 quickly eliminates any acetaldehyde produced from the break down of alcohol. However, some people have an inactive form of the ALDH2 protein. When these people drink alcohol, their bodies cannot get rid of the acetaldehyde and as a result, it builds up. This increases its toxic and mutation-causing capabilities. People from eastern Asia are most likely to have the inactive form of ALDH2 and are more vulnerable to developing alcohol-induced cancer.
What happens when someone stops drinking alcohol?
Compared to those who continue to drink alcohol, people who quit drinking lower their risk of developing cancers of the respiratory and digestive systems. After 20 years of not drinking, former drinkers can even reduce their risk for cancer to the level of risk seen in those who never consumed alcohol.
What if someone is already diagnosed with cancer, but continues to drink alcohol? What about cancer survivors who drink alcohol?
Between one-in-three and one-in-two patients who have been diagnosed with a cancer of the respiratory/digestive systems continue to drink alcohol. A study involving nearly 210,000 cancer survivors found that high alcohol consumers had an 8% greater chance of death and 17% greater risk for cancer recurrence compared to those who rarely or never drank alcohol.
People who consume alcohol after a diagnosis of respiratory/digestive cancer are at increased risk of developing additional cancers. Stopping alcohol consumption can reduce this risk.
Women who have estrogen receptor positive breast cancer who consume more than 7 drinks per week have a 90% greater risk of developing an additional breast cancer compared to non-drinkers. Patients with breast cancer who drink more than 7 drinks per week also develop other new cancers, including colorectal cancer. Moderate or heavy levels of drinking also increases the risk of breast cancer recurrence and death.
Abusing alcohol and excessive drinking can reduce the success of cancer treatments and can complicate the patient’s health with longer stays in the hospital, more surgeries, delayed recovery, greater risk of death and higher healthcare costs. The patient’s response to treatment may be further complicated by nutritional deficiencies, lowered immunity and heart problems that can arise due to alcohol abuse.
- 1 Urry, L. A., Cain, M. L., Wasserman, S. A., Minorsky, P. V., & Reece, J. B. (2017). Campbell Biology (11th ed.). Pearson.
- 2ab Alberts, B., Johnson, A., Lewis, J., Raff, M., Roberts, K., & Walter, P. Molecular Biology of the Cell; Fourth Edition. 23. Cancer. Garland Science; NY. 2002.
- 3 Kehe K, Szinicz L. "Medical aspects of sulphur mustard poisoning." Toxicology. 2005 Oct 30;214(3):198-209. [PUBMED]
- 4ab Robert A. Weinberg. "The Roots of Human Cancer." Bulletin of the American Academy of Arts and Sciences, Vol. 41, No. 8 (May, 1988), pp. 28-36 [http://www.jstor.org/sici?sici=0002-712X(198805)41%3A8%3C28%3ATROHC%3E2.0.CO%3B2-6]
- 5 Murugavel KG, Naranatt PP, Shankar EM, Mathews S, Raghuram K, Rajasambandam P, Jayanthi V, Surendran R, Murali A, Srinivas U, Palaniswamy KR, Srikumari D, Thyagarajan SP."Prevalence of aflatoxin B1 in liver biopsies of proven hepatocellular carcinoma in India determined by an in-house immunoperoxidase test." J Med Microbiol. 2007 Nov;56(Pt 11):1455-9. [PUBMED]
- 6 Eberle CE, Sandler DP, Taylor KW, White AJ. Hair dye and chemical straightener use and breast cancer risk in a large US population of black and white women [published online ahead of print, 2019 Dec 3]. Int J Cancer. 2019;10.1002/ijc.32738. doi:10.1002/ijc.32738 [PUBMED]
- 7 Cohen I."Aromatase inhibitors and the endometrium." Maturitas. 2008 Apr 28. [PUBMED]
- 8 Ciocca DR, Fanelli MA."Estrogen receptors and cell proliferation in breast cancer." Trends Endocrinol Metab. 1997 Oct;8(8):313-21. [PUBMED]
- 9ab Anderson LM. Environmental genotoxicants/carcinogens and childhood cancer: filling knowledge gaps. Curr Probl Pediatr Adolesc Health Care. 2008 Feb;38(2):50-63. [PUBMED]
- 10ab Williams JH, Phillips TD, Jolly PE, Stiles JK, Jolly CM, Aggarwal D. Human aflatoxicosis in developing countries: a review of toxicology, exposure, potential health consequences, and interventions. The American Journal of Clinical Nutrition (2004). 80: 1106-1122. [PUBMED]
- 11 Bialecki ES, Di Bisceglie AM. Clinical presentation and natural course of hepatocellular carcinoma. European Journal of Gastroenterology and Hepatology (2005). 17: 485-489. [PUBMED]
- 12 Thomas MB. Hepatocellular carcinoma: The need for progress. Journal of Clinical Oncology (2005). 23: 2892-2899. [PUBMED]
- 13 Nobel Prize Presentation Speech by Professor W. Wernstedt, Dean of the Royal Caroline Institute, December 10, 1927. Accessed 6/8/10 [http://nobelprize.org/nobel_prizes/medicine/laureates/1926/press.html]
- 14 Benamrouz S, Conseil V, Creusy C, Calderon E, Dei-Cas E, Certad G. Parasites and malignancies, a review, with emphasis on digestive cancer induced by Cryptosporidium parvum (Alveolata: Apicomplexa). Parasite. 2012 May;19(2):101-15. Epub 2012 Feb 1. [PUBMED]
- 15 Fried B, Reddy A, Mayer D. Helminths in human carcinogenesis. Cancer Lett. 2011 Jun 28;305(2):239-49. Epub 2010 Jul 27. [PUBMED]
- 16ab Selgrad M, Malfertheiner P, Fini L, Goel A, Boland CR, Ricciardiello L. The role of viral and bacterial pathogens in gastrointestinal cancer. J Cell Physiol. 2008 Mar 12 . [PUBMED]
- 17 Zhu Y, Michelle Luo T, Jobin C, Young HA. Gut microbiota and probiotics in colon tumorigenesis. Cancer Lett. 2011 Oct 28;309(2):119-27. Epub 2011 Jun 24. [PUBMED]
- 18 Macdonald RS, Wagner K. Influence of Dietary Phytochemicals and Microbiota on Colon Cancer Risk. J Agric Food Chem. 2012 May 31. [Epub ahead of print] [PUBMED]
- 19 Bassaganya-Riera J, Viladomiu M, Pedragosa M, De Simone C, Hontecillas R. Immunoregulatory mechanisms underlying prevention of colitis-associated colorectal cancer by probiotic bacteria. PLoS One. 2012;7(4):e34676. Epub 2012 Apr 12. [PUBMED]
- 20 McLaughlin-Drubin ME, Meyers J, Munger K. Cancer associated human papillomaviruses. Curr Opin Virol. 2012 Jun 1. [Epub ahead of print] [PUBMED]
- 21ab Chaturvedi AK. Beyond cervical cancer: burden of other HPV-related cancers among men and women. J Adolesc Health. 2010 Apr;46(4 Suppl):S20-6. [PUBMED]
- 22 Gallo RC. Research and discovery of the first human cancer virus, HTLV-1. Best Pract Res Clin Haematol. 2011 Dec;24(4):559-65. doi: 10.1016/j.beha.2011.09.012. Epub 2011 Nov 16. [PUBMED]
- 23 Braoudaki M, Tzortzatou-Stathopoulou F. Tumorigenesis related to retroviral infections. J Infect Dev Ctries. 2011 Nov 15;5(11):751-8. [PUBMED]
- 24 Pichler K, Kattan T, Gentzsch J, Kress AK, Taylor GP, Bangham CR, Grassmann R."Strong induction of 4-1BB, a growth and survival promoting costimulatory receptor, in HTLV-1-infected cultured and patients' T cells by the viral Tax oncoprotein." Blood. 2008 May 1;111(9):4741-51. [PUBMED]
- 25 Brady G, MacArthur GJ, Farrell PJ. Epstein-Barr virus and Burkitt lymphoma. J Clin Pathol. 2007 Dec;60(12):1397-402. [PUBMED]
- 26 Shah KM, Young LS. Epstein-Barr virus and carcinogenesis: beyond Burkitt's lymphoma. Clin Microbiol Infect. 2009 Nov;15(11):982-8. [PUBMED]
- 27 Leonardi GC, Candido S, Cervello M, Nicolosi D, Raiti F, Travali S, Spandidos DA, Libra M. The tumor microenvironment in hepatocellular carcinoma (review). Int J Oncol. 2012 Jun;40(6):1733-47. doi: 10.3892/ijo.2012.1408. Epub 2012 Mar 22. [PUBMED]
- 28 Arora A, Chiao E, Tyring SK. AIDS malignancies. Cancer Treat Res. 2007;133:21-67. [PUBMED]
- 29 Flegal, Katherine M., Deanna Kruszon-Moran, Margaret D. Carroll, Cheryl D. Fryar, and Cynthia L. Ogden. "Trends in Obesity Among Adults in the United States, 2005 to 2014." Jama 315.21 (2016). [http://www.ncbi.nlm.nih.gov/pubmed/27272580] [PUBMED]
- 30 Ogden, Cynthia L., Margaret D. Carroll, Hannah G. Lawman, Cheryl D. Fryar, Deanna Kruszon-Moran, Brian K. Kit, and Katherine M. Flegal. "Trends in Obesity Prevalence Among Children and Adolescents in the United States, 1988-1994 Through 2013-2014." The Journal of the American Medical Association 315.21 (2016). [http://jama.jamanetwork.com/article.aspx?articleID=2526638]
- 31 Zylke, Jody W., and Howard Bauchner. "The Unrelenting Challenge of Obesity." Jama 315.21 (2016): 2277. [http://jama.jamanetwork.com/article.aspx?articleID=2526613]
- 32abc Al-Kalbani, Moza, and Ikram Burney. "The Epidemics of Obesity and Cancer: No Simple Remedy." Sultan Qaboos University Medical Journal 14.3 (2014): 294-96. [http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4117652/]
- 33abc Kruijsdijk, R. C.m. Van, E. Van Der Wall, and F. L.j. Visseren. "Obesity and Cancer: The Role of Dysfunctional Adipose Tissue." Cancer Epidemiology Biomarkers & Prevention (2009): 2569-578. [https://www.ncbi.nlm.nih.gov/pubmed/19755644] [PUBMED]
- 34ab Vucenik, Ivana, and Joseph P. Stains. "Obesity and Cancer Risk: Evidence, Mechanisms, and Recommendations." Annals of the New York Academy of Sciences 1271.1 (2012): 37-43. [http://www.ncbi.nlm.nih.gov/pubmed/23050962] [PUBMED]
- 35ab Doyle, Suzanne L., Claire L. Donohoe, Joanne Lysaght, and John V. Reynolds. "Visceral Obesity, Metabolic Syndrome, Insulin Resistance and Cancer." Proceedings of the Nutrition Society 71.1 (2011): 181-89. [http://www.ncbi.nlm.nih.gov/pubmed/22051112] [PUBMED]
- 36 Hursting, Stephen D., and Sarah M. Dunlap. "Obesity, Metabolic Dysregulation, and Cancer: A Growing Concern and an Inflammatory (and Microenvironmental) Issue." Annals of the New York Academy of Sciences 1271.1 (2012): 82-87. [http://www.ncbi.nlm.nih.gov/pubmed/23050968] [PUBMED]
- 37 Percik, R., and M. Stumvoll. "Obesity and Cancer." Experimental and Clinical Endocrinology & Diabetes 117.10 (2009): 563-66. [http://www.ncbi.nlm.nih.gov/pubmed/19924603] [PUBMED]
- 38 Taliaferro-Smith, L., A. Nagalingam, B. Knight, E. Oberlick, N. Saxena, and D. Sharma. "Integral Role of PTP1B in Adiponectin-mediated Inhibition of Oncogenic Actions of Leptin in Breast Carcinogenesis." Neoplasia 15.1 (2013): 23-38. [https://www.ncbi.nlm.nih.gov/pubmed/?term=integral+role+of+PTP1B+in+adiponectin-mediated+inhibition+of+oncogenic+actions] [PUBMED]
- 39 Saxena, Neeraj K., and Dipali Sharma. "Metastasis Suppression by Adiponectin." Cell Adhesion & Migration 4.3 (2010): 358-62. [http://www.ncbi.nlm.nih.gov/pubmed/20418665] [PUBMED]
- 40 Siveen, Kodappully Sivaraman, Sakshi Sikka, Rohit Surana, Xiaoyun Dai, Jingwen Zhang, Alan Prem Kumar, Benny K.h. Tan, Gautam Sethi, and Anupam Bishayee. "Targeting the STAT3 Signaling Pathway in Cancer: Role of Synthetic and Natural Inhibitors." Biochimica Et Biophysica Acta (BBA) - Reviews on Cancer 1845.2 (2014): 136-54. [http://www.ncbi.nlm.nih.gov/pubmed/24388873] [PUBMED]
- 41 Fujimoto, Hiroshi, Takafumi Sangai, Genichiro Ishii, Akashi Ikehara, Takeshi Nagashima, Masaru Miyazaki, and Atsushi Ochiai. "Stromal MCP-1 in Mammary Tumors Induces Tumor-associated Macrophage Infiltration and Contributes to Tumor Progression." International Journal of Cancer Int. J. Cancer 125.6 (2009): 1276-284. [http://www-ncbi-nlm-nih-gov.proxy.library.emory.edu/pubmed/19479998] [PUBMED]
- 42 Harvey, Alison E., Laura M. Lashinger, and Stephen D. Hursting. "The Growing Challenge of Obesity and Cancer: An Inflammatory Issue." Annals of the New York Academy of Sciences 1229.1 (2011): 45-52. [http://www.ncbi.nlm.nih.gov/pubmed/21793838] [PUBMED]
- 43 Wu, Y., and B. P. Zhou. "TNF-¿/NF-¿B/Snail Pathway in Cancer Cell Migration and Invasion." Br J Cancer British Journal of Cancer 102.4 (2010): 639-44. [http://www-ncbi-nlm-nih-gov.proxy.library.emory.edu/pubmed/20087353] [PUBMED]
- 44abc Nishimoto, S., D. Fukuda, Y. Higashikuni, K. Tanaka, Y. Hirata, C. Murata, J.-R. Kim-Kaneyama, F. Sato, M. Bando, S. Yagi, T. Soeki, T. Hayashi, I. Imoto, H. Sakaue, M. Shimabukuro, and M. Sata. "Obesity-induced DNA Released from Adipocytes Stimulates Chronic Adipose Tissue Inflammation and Insulin Resistance." Science Advances 2.3 (2016). [http://www.ncbi.nlm.nih.gov/pubmed/?term=10.1126%2Fsciadv.1501332] [PUBMED]
- 45ab Wang, Xuyi, Evan R. Simpson, and Kristy A. Brown. "Aromatase Overexpression in Dysfunctional Adipose Tissue Links Obesity to Postmenopausal Breast Cancer." The Journal of Steroid Biochemistry and Molecular Biology 153 (2015): 35-44. PubMed. [http://www.ncbi.nlm.nih.gov/pubmed/26209254] [PUBMED]
- 46 Wang, D., and R. N. Dubois. Prostaglandins and Cancer. Gut 55.1 (2006): 115-22. [http://www.ncbi.nlm.nih.gov/pubmed/16118353] [PUBMED]
- 47 Subbaramaiah, K., P. G. Morris, X. K. Zhou, M. Morrow, B. Du, D. Giri, L. Kopelovich, C. A. Hudis, and A. J. Dannenberg. "Increased Levels of COX-2 and Prostaglandin E2 Contribute to Elevated Aromatase Expression in Inflamed Breast Tissue of Obese Women." Cancer Discovery 2.4 (2012): 356-65. [http://www.ncbi.nlm.nih.gov/pubmed/22576212] [PUBMED]
- 48 Grundy, Scott M. Metabolic Syndrome Update. Trends in Cardiovascular Medicine 26.4 (2016). [http://www.ncbi.nlm.nih.gov/pubmed/26654259] [PUBMED]
- 49 Gallagher, E. J., and D. LeRoith. "Minireview: IGF, Insulin, And Cancer." Endocrinology 152.7 (2011): 2546-551. [http://www.ncbi.nlm.nih.gov/pubmed/21540285] [PUBMED]
- 50 Djiogue, S., A. H. Nwabo Kamdje, L. Vecchio, M. J. Kipanyula, M. Farahna, Y. Aldebasi, and P. F. Seke Etet. Insulin Resistance and Cancer: The Role of Insulin and IGFs. Endocrine Related Cancer 20.1 (2012). [http://www.ncbi.nlm.nih.gov/pubmed/23207292] [PUBMED]
- 51abc Arcidiacono, Biagio, Stefania Iiritano, Aurora Nocera, Katiuscia Possidente, Maria T. Nevolo, Valeria Ventura, Daniela Foti, Eusebio Chiefari, and Antonio Brunetti. Insulin Resistance and Cancer Risk: An Overview of the Pathogenetic Mechanisms. Experimental Diabetes Research 2012 (2012): 1-12. [http://www.ncbi.nlm.nih.gov/pubmed/22701472] [PUBMED]
- 52 Shaw, Leslie M. The Insulin Receptor Substrate (IRS) Proteins. Cell Cycle 10.11 (2011): 1750-756. [PUBMED]
- 53 Lee, Byung-Cheol, and Jongsoon Lee. "Cellular and Molecular Players in Adipose Tissue Inflammation in the Development of Obesity-induced Insulin Resistance." Biochimica Et Biophysica Acta (BBA) - Molecular Basis of Disease 1842.3 (2014): 446-62. [http://www.ncbi.nlm.nih.gov/pubmed/23707515] [PUBMED]
- 54 Parekh, Parth J., Luis A. Balart, and David A. Johnson. "The Influence of the Gut Microbiome on Obesity, Metabolic Syndrome and Gastrointestinal Disease." Clinical and Translational Gastroenterology Clin Trans Gastroenterol 6.6 (2015). [http://www.ncbi.nlm.nih.gov/pubmed/26087059] [PUBMED]
- 55abc Rogers, Connie J., Kumble Sandeep Prabhu, and Matam Vijay-Kumar. "The Microbiome and Obesity¿An Established Risk for Certain Types of Cancer." The Cancer Journal 20.3 (2014): 176-80. [http://www.ncbi.nlm.nih.gov/pubmed/24855004] [PUBMED]
- 56abcd Shen, Jian, Martin S. Obin, and Liping Zhao. "The Gut Microbiota, Obesity and Insulin Resistance." Molecular Aspects of Medicine 34.1 (2013): 39-58. [http://www.ncbi.nlm.nih.gov/pubmed/23159341] [PUBMED]
- 57ab Caricilli, Andrea M., and Mario J.a. Saad. "Gut Microbiota Composition and Its Effects on Obesity and Insulin Resistance." Current Opinion in Clinical Nutrition and Metabolic Care 17.4 (2014): 312-18. [http://www.ncbi.nlm.nih.gov/pubmed/24848531] [PUBMED]
- 58ab Manco, Melania, Lorenza Putignani, and Gian Franco Bottazzo. "Gut Microbiota, Lipopolysaccharides, and Innate Immunity in the Pathogenesis of Obesity and Cardiovascular Risk." Endocrine Reviews 31.6 (2010): 817-44. [http://www.ncbi.nlm.nih.gov/pubmed/20592272] [PUBMED]
- 59 Perry, Rachel J., Liang Peng, Natasha A. Barry, Gary W. Cline, Dongyan Zhang, Rebecca L. Cardone, Kitt Falk Petersen, Richard G. Kibbey, Andrew L. Goodman, and Gerald I. Shulman. "Acetate Mediates a Microbiome¿brain¿ß-cell Axis to Promote Metabolic Syndrome." Nature 534.7606 (2016): 213-17. [http://www.ncbi.nlm.nih.gov/pubmed/27279214] [PUBMED]
- 60abc Fukumura, Dai, Joao Incio, Ram C. Shankaraiah, and Rakesh K. Jain. "Obesity and Cancer: An Angiogenic and Inflammatory Link." Microcirculation 23.3 (2016): 191-206. [http://www.ncbi.nlm.nih.gov/pubmed/26808917] [PUBMED]
- 61 Guiu, B., J. M. Petit, F. Bonnetain, S. Ladoire, S. Guiu, J.-P. Cercueil, D. Krause, P. Hillon, C. Borg, B. Chauffert, and F. Ghiringhelli. "Visceral Fat Area Is an Independent Predictive Biomarker of Outcome after First-line Bevacizumab-based Treatment in Metastatic Colorectal Cancer." Gut 59.3 (2009): 341-47. [http://www.ncbi.nlm.nih.gov/pubmed/19837679] [PUBMED]
- 62 Osman, Mohammed, and Bryan Hennessy. "Obesity Correlation With Metastases Development and Response to First-Line Metastatic Chemotherapy in Breast Cancer." Clinical Medicine Insights: Oncology CMO (2015): 105. [http://www.ncbi.nlm.nih.gov/pubmed/26628862] [PUBMED]
- 63 Chen, Sheng, Can-Ming Chen, Ying Zhou, Ruo-Ji Zhou, Ke-Da Yu, and Zhi-Ming Shao. "Obesity or Overweight Is Associated with Worse Pathological Response to Neoadjuvant Chemotherapy among Chinese Women with Breast Cancer." PLoS ONE 7.7 (2012) [http://www.ncbi.nlm.nih.gov/pubmed/22848477] [PUBMED]
- 64 Incio, J., H. Liu, P. Suboj, S. M. Chin, I. X. Chen, M. Pinter, M. R. Ng, H. T. Nia, J. Grahovac, S. Kao, S. Babykutty, Y. Huang, K. Jung, N. N. Rahbari, X. Han, V. P. Chauhan, J. D. Martin, J. Kahn, P. Huang, V. Desphande, J. Michaelson, T. P. Michelakos, C. R. Ferrone, R. Soares, Y. Boucher, D. Fukumura, and R. K. Jain. "Obesity-induced Inflammation and Desmoplasia Promote Pancreatic Cancer Progression and Resistance to Chemotherapy." Cancer Discovery (2016) [http://www.ncbi.nlm.nih.gov/pubmed/27246539] [PUBMED]
- 65 Merika, E. E., K. N. Syrigos, and M. W. Saif. "Desmoplasia in Pancreatic Cancer. Can We Fight It?" Gastroenterology Research and Practice 2012 (2012): 1-10. [http://www.ncbi.nlm.nih.gov/pubmed/23125850] [PUBMED]
- 66 Chen, Jiezhong, Xu-Feng Huang, Liang Qiao, and Andrew Katsifis. "Insulin Caused Drug Resistance to Oxaliplatin in Colon Cancer Cell Line HT29." Journal of Gastrointestinal Oncology 2.1 (2011): 27-33. [http://www.ncbi.nlm.nih.gov/pubmed/22811824] [PUBMED]
- 67abcd Griggs, J. J., P. B. Mangu, H. Anderson, E. P. Balaban, J. J. Dignam, W. M. Hryniuk, V. A. Morrison, T. M. Pini, C. D. Runowicz, G. L. Rosner, M. Shayne, A. Sparreboom, L. E. Sucheston, and G. H. Lyman. "Appropriate Chemotherapy Dosing for Obese Adult Patients With Cancer: American Society of Clinical Oncology Clinical Practice Guideline." Journal of Clinical Oncology 30.13 (2012): 1553-561. [http://www.ncbi.nlm.nih.gov/pubmed/22473167] [PUBMED]
- 68abc Lyman, Gary H., and Alex Sparreboom. "Chemotherapy Dosing in Overweight and Obese Patients with Cancer." Nature Reviews Clinical Oncology Nat Rev Clin Oncol 10.8 (2013): 451-59. [http://www.ncbi.nlm.nih.gov/pubmed/23856744] [PUBMED]
- 69ab Hourdequin, K. C., W. L. Schpero, D. R. Mckenna, B. L. Piazik, and R. J. Larson. "Toxic Effect of Chemotherapy Dosing Using Actual Body Weight in Obese versus Normal-weight Patients: A Systematic Review and Meta-analysis." Annals of Oncology 24.12 (2013): 2952-962. [http://www.ncbi.nlm.nih.gov/pubmed/23965736] [PUBMED]
- 70 Allavena P, Garlanda C, Borrello MG, Sica A, Mantovani A. Pathways connecting inflammation and cancer. Curr Opin Genet Dev. 2008 Mar 4. [PUBMED]
- 71 Lisa M. Coussens & Zena Werb. Inflammation and cancer. Nature (420). December 2002. [http://osteosarcomasupport.org/immunology/inflammation-cancer-nature-2002.pdf]
- 72 Zeiger E. The test that changed the world: The Ames test and the regulation of chemicals. Mutat Res. 2019;841:43–48. doi:10.1016/j.mrgentox.2019.05.007 [PUBMED]
- 73 Vogt PK. Cancer genes. West J Med. 1993;158(3):273–278. [PUBMED]
- 74 Hanahan D, Weinberg RA. The hallmarks of cancer. Cell. 2000;100(1):57–70. [PUBMED] doi:10.1016/s0092-8674(00)81683-9
- 75 Report on Carcinogens, Fourteenth Edition; U.S. Department of Health and Human Services, Public Health Service, National Toxicology Program. accessed 12/20/19. [https://ntp.niehs.nih.gov/whatwestudy/assessments/cancer/roc/index.html]
- 76 Weinberg, RA. "Finding the Anti-Oncogene." Scientific American (1988). 259(3): 44-51. [PUBMED]
- 77 Ke Q, Ellen TP, Costa M. Nickel compounds induce histone ubiquitination by inhibiting histone deubiquitinating enzyme activity. Toxicol Appl Pharmacol. 2007 Dec 23. [PUBMED]
- 78 Nicotiana Tabacum [http://eol.org/pages/581050/overview]
- 79 Nicotiana Tabacum L. Cultivated Tobacco. USDA Natural Resources Conservation Service. [http://plants.usda.gov/core/profile?symbol=NITA&mapType=nativity]
- 80ab Nicotine and Tobacco. Medline Plus. [http://www.nlm.nih.gov/medlineplus/ency/article/000953.htm]
- 81 Leary, Warren E. Cigarette Company Developed Tobacco With Stronger Nicotine; Head of F.D.A. Tells of Chemical Manipulation. NY Times Archives. [http://www.nytimes.com/1994/06/22/us/cigarette-company-developed-tobacco-with-stronger-nicotine-head-fda-tells.html]
- 82abcdefghij Proctor RN. Tobacco and the global lung cancer epidemic. Nat Rev Cancer. 2001 Oct;1(1):82-6. [PUBMED]
- 83 Inside The Tobacco Deal. Frontline. Public Broadcasting Service (PBS). [http://www.pbs.org/wgbh/pages/frontline/shows/settlement/timelines/fullindex.html]
- 84 Master Settlement Agreement. Washington State Office of the Attorney General. [https://www.atg.wa.gov/master-settlement-agreement]
- 85ab E-Cigarette History. Consumer Advocates for Smoke-free Alternatives Association. [http://casaa.org/E-cigarette_History.html]
- 86 CVS Caremark to Stop Selling Tobacco at all CVS/pharmacy Locations. CVS Press Releases. CVS Caremark. Accessed 12-2-19 [https://cvshealth.com/newsroom/press-releases/cvs-caremark-stop-selling-tobacco-all-cvspharmacy-locations]
- 87ab FDA's Deeming Regulations for E-Cigarettes, Cigars, and All Other Tobacco Products. FDA website. Accessed 1-1-2020 [View the FDA site]
- 88 What's in a Cigarette? American Lung Association. [http://www.lung.org/stop-smoking/about-smoking/facts-figures/whats-in-a-cigarette.html]
- 89 Cigar Smoking and Cancer. National Cancer Institute. [http://www.cancer.gov/cancertopics/factsheet/Tobacco/cigars]
- 90 An Emerging Deadly Trend: Waterpipe Tobacco Use. Tobacco Policy Project. American Lung Association. [http://www.lungusa2.org/embargo/slati/Trendalert_Waterpipes.pdf]
- 91 Hookah Smoking: A Growing Threat to Public Health Issue Brief. Smokefree Communities Project. American Lung Association. [http://www.lung.org/stop-smoking/tobacco-control-advocacy/reports-resources/cessation-economic-benefits/reports/hookah-policy-brief.pdf]
- 92 Cobb C, Ward KD, Maziak W, Shihadeh AL, Eissenberg T. Waterpipe tobacco smoking: an emerging health crisis in the United States. Am J Health Behav. 2010 May-Jun;34(3):275-85. [PUBMED]
- 93 Rezk-Hanna M, Doering L, Robbins W, Sarna L, Elashoff RM, Victor RG. Acute Effect of Hookah Smoking on Arterial Stiffness and Wave Reflections in Adults Aged 18 to 34 Years of Age. Am J Cardiol. 2018 Jun 5. pii: S0002-9149(18)31206-2. doi: 10.1016/j.amjcard.2018.05.033. [PUBMED]
- 94 Health Risks of Waterpipes, Smokeless Tobacco, and E-cigarettes. Cancer.Net. [http://www.cancer.net/navigating-cancer-care/prevention-and-healthy-living/tobacco-use/health-risks-waterpipes-smokeless-tobacco-and-e-cigarettes]
- 95 Electronic Cigarettes (e-Cigarettes). U.S. Food and Drug Administration. [http://www.fda.gov/newsevents/publichealthfocus/ucm172906.htm]
- 96 Adam M. Leventhal, David R. Strong, Matthew G. Kirkpatrick, Jennifer B. Unger, Steve Sussman, Nathaniel R. Riggs, Matthew D. Stone, Rubin Khoddam, Jonathan M. Samet, Janet Audrain-McGovern. Association of Electronic Cigarette Use With Initiation of Combustible Tobacco Product Smoking in Early Adolescence.
- 97 Restrict the Sale of Electronic Cigarettes. American Cancer Society. [http://www.cancer.org/myacs/eastern/areahighlights/cancernynj-news-ny-ecig-health-vote]
- 98 E-cigarettes ‘Potentially as Harmful as Tobacco Cigarettes’. UCONN Today. 2017 Jun 12. [UCONN Today]
- 99 Cossio R, Cerra ZA, Tanaka H. Vascular effects of a single bout of electronic cigarette use. Clin Exp Pharmacol Physiol. 2020;47(1):3–6. doi:10.1111/1440-1681.13180 [PubMed]]
- 100 E-CIGARETTES LINKED TO INCREASED ARTERIAL STIFFNESS, BLOOD PRESSURE AND HEART RATE IN HUMANS. ELF 2017 Accessed 1-2-2020 Website]
- 101 Franzen KF, Willig J, Cayo Talavera S, et al. E-cigarettes and cigarettes worsen peripheral and central hemodynamics as well as arterial stiffness: A randomized, double-blinded pilot study. Vasc Med. 2018;23(5):419–425. doi:10.1177/1358863X18779694 [PubMed]
- 102abcde Boffetta P, Hecht S, Gray N, Gupta P, Straif K. Smokeless tobacco and cancer. Lancet Oncol. 2008 Jul;9(7):667-75. [PUBMED]
- 103abcdef Smokeless Tobacco. American Cancer Society. [http://www.cancer.org/cancer/cancercauses/tobaccocancer/smokeless-tobacco]
- 104 Centers for Disease Control and Prevention- Reports of the Surgeon General. U.S. Department of Health and Human Services. Accessed 1-2-2020 [View 2014 Progress Report]
- 105 Current Cigarette Smoking Among Adults - United States, 2005-2012. Morbidity and Mortality Weekly Report. Centers for Disease Control and Prevention. [http://www.cdc.gov/mmwr/pdf/wk/mm6302.pdf]
- 106ab Let's Make the Next Generation Tobacco-Free. Surgeon General's Report. U.S. Department of Health and Human Services. [http://www.surgeongeneral.gov/library/reports/50-years-of-progress/consumer-guide.pdf]
- 107 Heart Disease and Stroke. Centers for Disease Control and Prevention. [http://www.cdc.gov/tobacco/basic_information/health_effects/heart_disease/]
- 108 Just M, Ribera M, Monsó E, Lorenzo JC, Ferrándiz C. Effect of smoking on skin elastic fibres: morphometric and immunohistochemical analysis. Br J Dermatol. 2007 Jan;156(1):85-91. [PUBMED]
- 109ab COPD: Learn More Breathe Better. National Heart, Lung, and Blood Institute. [http://www.nhlbi.nih.gov/health/public/lung/copd/campaign-materials/pub/copd-atrisk.pdf]
- 110 How Does COPD Affect Breathing? National Heart, Lung, and Blood Institute. [http://www.nhlbi.nih.gov/health/public/lung/copd/what-is-copd/how-does-copd-affect-breathing.htm]
- 111 What is COPD? National Heart, Lung, and Blood Institute. [http://www.nhlbi.nih.gov/health/health-topics/topics/copd/]
- 112ab You Can Control Your Asthma. Centers for Disease Control and Prevention. [http://www.cdc.gov/asthma/pdfs/asthma_brochure.pdf]
- 113 Dumanski JP, Rasi C, Lonn M, Davies H, Ingelsson M, Giedraitis V, Lannfelt L, Magnusson PK, Lindgren CM, Morris AP, Cesarini D, Johannesson M, Tiensuu Janson E, Lind L, Pedersen NL, Ingelsson E, Forsberg LA. Smoking is associated with mosaic loss of chromosome Y. Science. 2014 Dec 4. pii: 1262092. [Epub ahead of print] [PUBMED]
- 114 Forsberg LA, Rasi C, Malmqvist N, Davies H, Pasupulati S, Pakalapati G, Sandgren J, Diaz de Stahl T, Zaghlool A, Giedraitis V, Lannfelt L, Score J, Cross NC, Absher D, Janson ET, Lindgren CM, Morris AP, Ingelsson E, Lind L, Dumanski JP. Mosaic loss of chromosome Y in peripheral blood is associated with shorter survival and higher risk of cancer. Nat Genet. 2014 Jun;46(6):624-8. doi: 10.1038/ng.2966. Epub 2014 Apr 28. [PUBMED]
- 115abcde Secondhand Smoke. American Cancer Society. [http://www.cancer.org/cancer/cancercauses/tobaccocancer/secondhand-smoke]
- 116abcd The Health Consequences of Involuntary Exposure to Tobacco Smoke: A Report of the Surgeon General. Publications and Reports of the Surgeon General. Office on Smoking and Health (US). Centers for Disease Control and Prevention (Atlanta, GA, US); 2006. [PUBMED]
- 117abcdefg Secondhand Smoke (SHS) Facts. Centers for Disease Control and Prevention. [http://www.cdc.gov/tobacco/data_statistics/fact_sheets/secondhand_smoke/general_facts/]
- 118 Vital Signs: Nonsmokers¿ Exposure to Secondhand Smoke ¿ United States, 1999-2008. Morbidity and Mortality Weekly Report. Centers for Disease Control and Prevention. [http://www.cdc.gov/mmwr/pdf/wk/mm5935.pdf]
- 119 Laubenthal J, Zlobinskaya O, Poterlowicz K, Baumgartner A, Gdula MR, Fthenou E, Keramarou M, Hepworth SJ, Kleinjans JC, van Schooten FJ, Brunborg G, Godschalk RW, Schmid TE, Anderson D. Cigarette smoke-induced transgenerational alterations in genome stability in cord blood of human F1 offspring. FASEB J. 2012 Oct;26(10):3946-56. Epub 2012 Jun 22. [PUBMED]
- 120 Zhang Y, Yang R, Burwinkel B, Breitling LP, Brenner H. F2RL3 methylation as a biomarker of current and lifetime smoking exposures. Environ Health Perspect. 2014 Feb;122(2):131-7. doi: 10.1289/ehp.1306937. Epub 2013 Nov 21. [PUBMED]
- 121 Marczylo EL, Amoako AA, Konje JC, Gant TW, Marczylo TH. Smoking induces differential miRNA expression in human spermatozoa: a potential transgenerational epigenetic concern? Epigenetics. 2012 May;7(5):432-9. doi: 10.4161/epi.19794. Epub 2012 May 1. [PUBMED]
- 122 Rehan VK, Liu J, Naeem E, Tian J, Sakurai R, Kwong K, Akbari O, Torday JS. Perinatal nicotine exposure induces asthma in second generation offspring. BMC Med. 2012 Oct 30;10:129. [PUBMED]
- 123 Rehan VK, Liu J, Sakurai R, Torday JS. Perinatal nicotine-induced transgenerational asthma. Am J Physiol Lung Cell Mol Physiol. 2013 Oct 1;305(7):L501-7. Epub 2013 Aug 2. [PUBMED]
- 124 New CDC study finds dramatic increase in e-cigarette-related calls to poison centers. CDC Newsroom Press Release. Centers for Disease Control and Prevention. [http://www.cdc.gov/media/releases/2014/p0403-e-cigarette-poison.html]
- 125 Richtel, Matt. Selling a Poison by the Barrel: Liquid Nicotine for E-Cigarettes. NY Times. [http://www.nytimes.com/2014/03/24/business/selling-a-poison-by-the-barrel-liquid-nicotine-for-e-cigarettes.html?_r=3]
- 126 Jane M. Garbutt, Whitney Miller, Sherry Dodd, Neil Bobenhouse, Randall Sterkel, Robert C. Strunk. Parental Use of Electronic Cigarettes.
- 127 FDA finalizes enforcement policy on unauthorized flavored cartridge-based e-cigarettes that appeal to children, including fruit and mint. FDA website. Accessed 1/2/2020[https://www.fda.gov/news-events/press-announcements/fda-finalizes-enforcement-policy-unauthorized-flavored-cartridge-based-e-cigarettes-appeal-children]
- 128 Electronic Cigarette Fires and Explosions. U.S. Fire Administration. FEMA. U.S. Department of Homeland Security. [https://www.usfa.fema.gov/downloads/pdf/publications/electronic_cigarettes.pdf]
- 129 "Man In Coma After E-Cig Blows Up In His Face". CBS Miami. [http://miami.cbslocal.com/2015/10/27/man-in-coma-after-e-cig-blows-up-in-his-face/]
- 130 "Electronic Cigarette Explodes in Man's Mouth, Burns His Face". The Huffington Post. [http://www.huffingtonpost.com/2012/02/16/electronic-cigarette-explode_n_1281707.html]
- 131 Lee M Jablow, Ryan J Sexton. Spontaneous Electronic Cigarette Explosion: A Case Report. American Journal of Medical Case Reports 3.4 (2015): 93-94.
- 132ab Tobacco-Related Mortality. Centers for Disease Control and Prevention. [http://www.cdc.gov/tobacco/data_statistics/fact_sheets/health_effects/tobacco_related_mortality/]
- 133abcdef The Health Consequences of Smoking¿50 Years of Progress: A Report of the Surgeon General. Reports of the Surgeon General. National Center for Chronic Disease Prevention and Health Promotion (US) Office on Smoking and Health. Atlanta (GA): Centers for Disease Control and Prevention (US); 2014. [PUBMED]
- 134 QuickStats: Number of Deaths from 10 Leading Causes-National Vital Statistics System, United States, 2010. Morbidity and Mortality Weekly Report. Centers for Disease Control and Prevention. [http://www.cdc.gov/mmwr/pdf/wk/mm6208.pdf]
- 135 Cancer Facts & Figures 2014. American Cancer Society. [http://www.cancer.org/acs/groups/content/@research/documents/webcontent/acspc-042151.pdf]
- 136 Michael Erikson, Judith Mackay, and Hana Ross. The Tobacco Atlas 4th edition. American Cancer Society. [http://www.tobaccoatlas.org/uploads/Images/PDFs/Tobacco_Atlas_2ndPrint.pdf]
- 137 Jha P, Ramasundarahettige C, Landsman V, Rostron B, Thun M, Anderson RN, McAfee T, Peto R. 21st-century hazards of smoking and benefits of cessation in the United States. N Engl J Med. 2013 Jan 24;368(4):341-50. [PUBMED]
- 138 How Tobacco Smoke Causes Disease: What It Means to You. Surgeon General's Report. U.S. Department of Health and Human Services. [http://www.cdc.gov/tobacco/data_statistics/sgr/2010/consumer_booklet/pdfs/consumer.pdf]
- 139 Max W, Sung HY, Shi Y. Deaths from secondhand smoke exposure in the United States: economic implications. Am J Public Health. 2012 Nov;102(11):2173-80. Epub 2012 Sep 20. [PUBMED]
- 140 Toll of Tobacco in the United States of America. Campaign for Tobacco-Free Kids. [http://www.tobaccofreekids.org/research/factsheets/pdf/0072.pdf]
- 141 Fast Facts. Centers for Disease Control and Prevention. [http://www.cdc.gov/tobacco/data_statistics/fact_sheets/fast_facts/]
- 142 Best Practices for Comprehensive Tobacco Control Programs-2014. Centers for Disease Control and Prevention. [http://www.cdc.gov/tobacco/stateandcommunity/best_practices/pdfs/2014/comprehensive.pdf]
- 143 The 1998 State Tobacco Settlement 15 Years Laters. Campaign for Tobacco-Free Kids. [https://www.tobaccofreekids.org/assets/content/what_we_do/state_local_issues/settlement/FY2014/StateSettlementReport_FY2014.pdf]
- 144ab Federal Trade Commission Cigarette Report for 2011. United States Federal Trade Commission. [http://www.ftc.gov/sites/default/files/documents/reports/federal-trade-commission-cigarette-report-2011/130521cigarettereport.pdf]
- 145abc Economic Facts About U.S. Tobacco Production and Use. Centers for Disease Control and Prevention. [http://www.cdc.gov/tobacco/data_statistics/fact_sheets/economics/econ_facts/]
- 146 Cigarette Consumption. Tobaccoatlas.org. [http://www.tobaccoatlas.org/uploads/Files/pdfs/products/cigarette_consumption/cigarette_consumption_pdf.pdf]
- 147ab Manufacturing Cigarettes. Tobaccoatlas.org. [http://www.tobaccoatlas.org/uploads/Files/pdfs/industry/manufacturing/manufacturing_pdf.pdf]
- 148ab Huang Yanzhong. E-Cigarettes: China's Next Growth Industry. Forbes. [http://www.forbes.com/sites/yanzhonghuang/2014/05/27/e-cigarettes-chinas-next-growth-industry/]
- 149ab Shu-Hong Zhu, Jessica Y Sun, Erika Bonnevie, Sharon E Cummins, Anthony Gamst, Lu Yin, Madeleine Lee. Four hundred and sixty brands of e-cigarettes and counting: implications for product regulation. Tob Control 2014;23:iii3-iii9. [http://tobaccocontrol.bmj.com/content/23/suppl_3/iii3.full.pdf+html]
- 150 Duke JC, Lee YO, Kim AE, Watson KA, Arnold KY, Nonnemaker JM, Porter L. Exposure to Electronic Cigarette Television Advertisements Among Youth and Young Adults. Pediatrics. 2014 Jun 2. pii: peds.2014-0269. [Epub ahead of print] [PUBMED]
- 151 Tomar SL, Alpert HR, Connolly GN. Patterns of dual use of cigarettes and smokeless tobacco among US males: findings from national surveys. Tob Control. 2010 Apr;19(2):104-9. Epub 2009 Dec 11. [PUBMED]
- 152ab Federal Trade Commission Smokeless Tobacco Report for 2011. United States Federal Trade Commission. [http://www.ftc.gov/sites/default/files/documents/reports/federal-trade-commission-smokeless-tobacco-report-2011/130521smokelesstobaccoreport.pdf]
- 153 TTB's Responsibilities - What We Do. Consumer Corner. Alcohol and Tobacco Tax Bureau. U.S. Department of the Treasury. [http://www.ttb.gov/consumer/responsibilities.shtml#Tobacco]
- 154 Legislation. Centers for Disease Control and Prevention. [http://www.cdc.gov/tobacco/data_statistics/by_topic/policy/legislation/]
- 155 Overview of the Family Smoking Prevention and Tobacco Control Act. Consumer Fact Sheet. Center for Tobacco Products. U.S. Food and Drug Administration. [http://www.fda.gov/downloads/TobaccoProducts/GuidanceComplianceRegulatoryInformation/UCM336940.pdf]
- 156 Tobacco Product Standard for Nicotine Level of Certain Products. https://www.reginfo.gov/public/do/eAgendaViewRule?pubId=202204&RIN=0910-AI76 Published Spring 2022. Accessed 08-11-2022
- 157 FDA Announces Plans for Proposed Rule to Reduce Addictiveness of Cigarettes and Other Combusted Tobacco Productshttps://www.fda.gov/news-events/press-announcements/fda-announces-plans-proposed-rule-reduce-addictiveness-cigarettes-and-other-combusted-tobacco US FDA News Release. Published online 06/21/2022 Accessed 08-11-2022
- 158ab Master Settlement Agreement. Washington State Office of the Attorney General. [http://www.atg.wa.gov/MSA.aspx#.U6HOCo1dVJ9]
- 159 Jones WJ, Silvestri GA. The Master Settlement Agreement and its impact on tobacco use 10 years later: lessons for physicians about health policy making. Chest. 2010 Mar;137(3):692-700. [PUBMED]
- 160 Loconte, Noelle K., et al. “Alcohol and Cancer: A Statement of the American Society of Clinical Oncology.” Journal of Clinical Oncology, vol. 36, no. 1, 2018, pp. 83–93. [PUBMED]