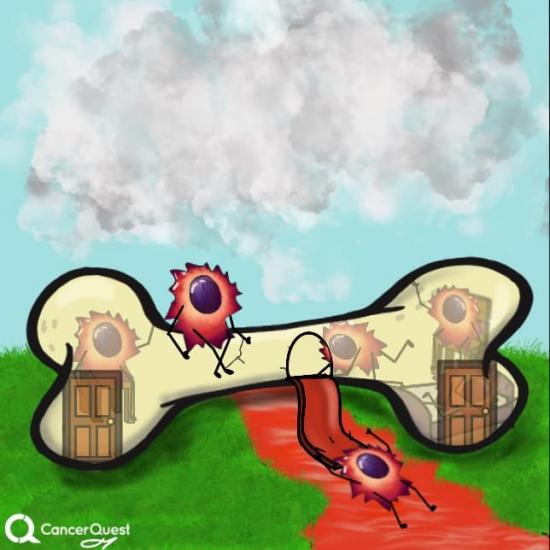
In hematopoietic stem cell transplantation, cancer cells living in the bone marrow are killed replaced with healthy stem cells.
Often, a combination of drugs and radiation is used to kill the cancer cells.

The new healthy cells move into the bone marrow and healthy blood cells are made.
The production of blood is called hematopoiesis (HEH-MAT-O-PO-E-SIS). The cells that divide and change (differentiate) to make our red and white blood cells are called hematopoietic stem cells (HSC). In adults, our blood cells come from our bones (in the bone marrow). When one of the cells that gives rise to these cells becomes cancerous, the defective bone marrow produces a mixture of healthy and cancerous cells. To eliminate the cancer, the defective bone marrow cells can be killed and replaced with normal cells.
There are two main ways in which normal stem cells are collected. In the first method stem cells are removed (harvested) from the bone marrow of the patient or a donor and given to the patient. This is called bone marrow transplantation (BMT) and it was developed first. In the second approach, HSC are removed blood taken from a donor - usually from an arm vein. The use of peripheral blood instead of marrow as a source of stem cells - called peripheral blood stem cell transplantation (PBSCT) came later. Both of these methods are ways of transferring healthy hematopoietic stem cells into patients - they are types of hematopoietic stem cell transplantation (HSCT).
The goal of both types of stem cell transplantation are the same. Only the source of the cells is different.
Hematopoietic Stem Cell Transplantation (HSCT)
Hematopoietic stem cell transplants (often referred to as 'stem cell transplants') are used to treat several types of cancer and is commonly used for leukemias, lymphomas and other blood cell cancers. BMT may also be used to treat patients with solid tumors. The following sections cover:
- The History of Bone Marrow Transplantation (BMT)
- Conditions Treated with Stem Cell Transplants
- Types of Stem Cell Transplant
- Qualifications for Transplant
- Preparation (Conditioning) for Transplant
- Donor Stem Cells Used in Transplants
- Graft Versus Host Disease (GVHD)
- Complications of Bone Marrow Transplant
The History of Bone Marrow Transplant (BMT)
Scientists in the mid 19th century proposed bone marrow was responsible for the formation of blood cells; this idea was later shown to be correct. The current belief is that all blood cells are actually formed by a small subset of bone marrow cells; these cells are called "hematopoietic stem cells"1 (because the cells used for transplantation are stem cells, this phrase will be used in the rest of this article). These hematopoietic stem cells live in the bone marrow and have special set of characteristics; they can renew themselves, they can develop into any type of blood cell and they leave the marrow to enter the blood and lymphatic systems. They should not be confused with embryonic stem cells, which are obtained from a developing fetus.
Early attempts to transplant stem cells were generally unsuccessful because the appropriate methods were not yet known. Marrow transplantation was further explored after World War II. The Atomic Energy Commission was concerned about the effects of atomic weapons, specifically the radiation to which combatants and civilians were exposed. Stem cells are especially sensitive to radiation and it was thought that transplantation could restore the function of damaged cells2. Today bone marrow transplantation is a viable option for many individuals. Because of continued research the success rate has steadily improved.3
Conditions Treated with Bone Marrow Transplant
Immune Cell and Inherited Disorders
Some children are born with an inability to make certain kinds of blood cells (lymphocytes), leaving them susceptible to life-threatening infections. These children can be treated with stem cell transplants. They have a good chance of successful transplant because their immune system is already deficient. This reduces the need for intensive pretreatment and the chance of rejection and graft versus host disease (GVHD, learn more) is much lower.
Children born with inherited blood disorders, such as sickle cell disease and thalassemia, are now considered for transplants. These conditions are generally not life-threatening and in the past bone marrow transplantation was considered too risky. Because of the advances and increased success rate of transplants this option is now available to these patients.
Leukemia, Lymphoma, Myeloma
Leukemia, lymphoma, and myeloma are the cancers that are most commonly treated with bone marrow transplants and stem cell transplantation. The following is a list of the subtypes of these cancers that are treated with BMT/HSCT:
- acute myelogenous leukemia4
- adult acute lymphocytic leukemia4
- childhood acute lymphocytic leukemia (very high risk, no remission, or relapse)4
- chronic lymphocytic leukemia4
- chronic myelogenous leukemia4
- Hodgkin lymphoma (if no longer responds to treatment or returns)4
- idiopathic myelofibrosis (agnogenic myeloid metaplasia)
- lymphoma (if refractory to treatment or recurrent)4
- myelodysplastic syndrome (oligoblastic myelogenous leukemia)4
- myeloma4
Types of Stem Cell Transplant
There are three types of stem cell transplant that differ in the source of the donor cells:
Autologous
Donor and recipient is the same individual1. Treatment for blood and marrow cancers can include large amounts of chemotherapy and radiation. These types of therapy can damage the marrow, resulting in very low blood cell production. Autologous transplant is used to restore the damaged marrow. During remission; stem cells are harvested after intensive therapy when very few cancerous cells remain. The stem cells are frozen for later use. This type of transplant will not result in rejection or graft versus host disease5.
Syngenic Transplantation
Donor and recipient are identical twins. Donor cells are not rejected and recipient tissue is not attacked by donor cells (no GVHD)6.
Allogenic Transplantation
Donor and recipient are two different individuals. There are two types of allogenic transplant; related allogenic and unrelated allogenic1. Related allogenic is usually a sibling. Unrelated allogenic is usually a closely matched individual from a donor list; this is often referred to as a 'matched unrelated donor' or MUD transplant7, 6.
Both unrelated and related allogenic transplant recipients face immune rejection of the donated cells and/or the possibility that the donated cells will attack recipient tissue (GVHD). To prevent these from occurring, allogenic transplant recipients must undergo a preparatory regimen called 'conditioning'1 (discussed below).
Qualifications for Transplant
To determine whether a transplant is appropriate, several factors are taken into account. These include (in no specific order):
Overall Health
Because stem cell transplants are very taxing on the body they are not usually done in patients that cannot handle the stresses involved.
Age of the Patient
Transplants are most often performed on younger patients because the procedure is physically demanding. Patients over the age of 50 are more likely to have complications, including graft-versus-host disease (GVHD)1. They are also less likely to tolerate the side effects of the conditioning regimen (learn about the conditioning regimen).
Medical Condition and Likelihood of Response
Although ongoing research and advances have increased the success of stem cell transplantation, it can still be a difficult procedure and should only be used when there is a strong likelihood of response1.
Availability of Donor Cells
This is the most important factor. If there are no available matching donor cells, then a transplant is not possible. When the patient is donating their own cells (autologous transplants) a sufficient amount of healthy cells must be available. For procedures in which the patient is NOT the donor (allogenic transplants), a close HLA match (discussed below) is necessary8. A close HLA match is defined as at least 5 out of 6 HLA markers matching for adults getting donor stem cells and 4 out of 6 for children getting stem cells from cord blood. These guidelines are set by the National Marrow Donor Program (an international organization).
Preparation (Conditioning) for Transplant
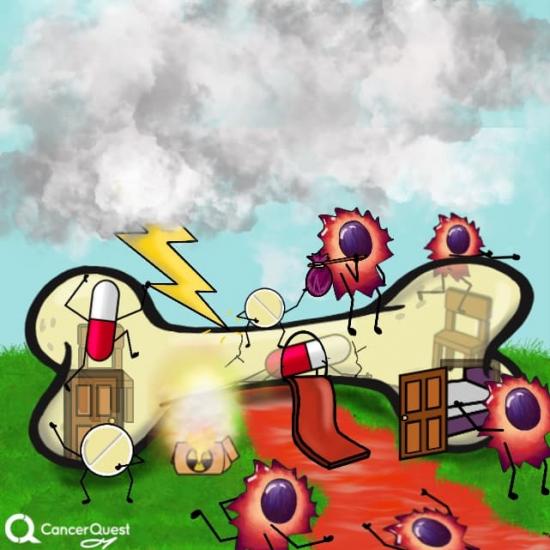
The conditioning regimen for patients undergoing an allogenic stem cell transplant is a difficult experience, but is absolutely necessary to produce a favorable outcome. Remember, stem cells are the mother cells of all the cells in the blood, including immune cells (white blood cells). If donor cells were infused into an individual with a functioning immune system a battle would be waged by the recipient immune system on the donor stem cells. This battle would destroy the donor cells, preventing them from taking hold and curing the disease. The conditioning regimen destroys the recipient immune cells providing an easier path for the donor cells2.
The conditioning regimen used varies by location and underlying condition being treated, but may include a combination of chemotherapy agents and total body irradiation (radiation therapy). Some centers use just chemotherapy, some use both chemotherapy and radiation. These therapies are especially deadly to the stem cells, damaging them so they can no longer produce many healthy cells. In general high amounts of chemotherapy and radiation in the conditioning program provide better remission rates2. Again, the conditioning regimen prepares the body to receive the donor cells in a way that will ease their journey and their establishment within the bone marrow of the recipient.
Conditioning begins the week before transplant. The days before transplant are labeled "day minus 8", "day minus 7", "day minus 6: etc; transplant day is "day zero"; and the days following transplant are "day plus 1", "day plus 2", etc.
Donor Cells Used in Hematopoietic Stem Cell Transplants
Donor Choice and Screening
Transplanted stem cells can come from the patient (autologous), an identical twin (syngenic), or a different individual (allogenic)1. In the case of allogenic transplant, siblings are the first choice for donor cells. When a sibling is unavailable or not a match donor cells are found from a marrow donor registry program8. These programs have lists of willing donors. For a donor to be considered they must match with the patient for at least 5 out of 6 HLA markers.
Before a stem cell donor is chosen, they must pass a thorough health exam9. This includes an electrocardiogram, chest x-ray, blood chemistry, and blood count. The donor is also tested for various viral infections including, hepatitis, human immunodeficiency virus (HIV), and cytomegalovirus (presence of antibodies to CMV does not necessarily exclude a person from being a donor)10.
There are three main sources of stem cells; donor bone marrow, donor blood, or cord blood11.
Donor Bone Marrow
Marrow donation is a surgical procedure, done in an operating room under general anesthesia. A needle is inserted through the skin and into the pelvic bone and marrow is removed. This procedure is repeated until several pints are removed. The donor remains in the hospital until they recover from the effects of anesthesia and pain11. The marrow is filtered, processed, and given to the recipient usually within 24 hours.
Donor Blood
Stem cells regularly leave the marrow and enter the bloodstream, but under normal conditions there are not enough of them (in the blood) for a successful transplant. Doctors can give a drug that encourages the stem cells to leave the marrow at a much higher rate. The drug is given to donors several days before the blood is collected. On collection day the donor undergoes apheresis11, a process where donor blood is passed through a machine that separates the blood into 4 components; blood plasma, red blood cells, white blood cells, and platelets (more about blood counts). The stem cells are located in the platelet and white blood cell components so they are kept, but the rest of the blood is put back into the donor's body.
Cord Blood
Cord blood is taken from the umbilical cord and placenta after childbirth. Children and small adults can receive a transplant with cord blood stem cells. The umbilical cord and attached placenta are drained immediately after childbirth and the cells are frozen for later use.12
Stem Cell Infusion
The infusion of stem cells into the cancer patient is similar to a regular blood transfusion. Stem cells are purified from blood taken from a donor and processed, they are ready to be given to the recipient. The cells are collected in a blood transfusion bag and infused intravenously (through a vein) either through an IV or a vascular access device (VAD). Infusions may last several hours and patients are checked for signs of a reaction. Signs of a reaction may include fever, chills, hives, a drop in blood pressure, shortness of breath, nausea, and headache. Reactions are rare and can usually be easily managed.
Graft Versus Host Disease (GVHD)
Graft-versus-host disease is a condition that can develop after allogenic stem cell transplant. It occurs when donor-derived T cells attack the recipient tissue13. There are two types of graft-versus host disease; acute GVHD (aGVHD) and chronic GVHD (cGVHD). The difference between acute and chronic disease is the time of onset after transplantation; aGVHD occurs before day 100 and cGVHD after day 100. This definition is not completely accurate. Acute symptoms may occur past day 100 and some patients may experience an overlap of symptoms. Acute and chronic GVHD are responsible for most of the complications of stem cell transplantation. It is extremely important to discuss any issues with a health care professional.
Although GVHD is thought of as a negative side-effect, low-grade GVHD is actually associated with a lower rate of relapse. This is due to what is called the graft-versus-malignancy effect, where the donor-derived T cells attack the malignant cells (leukemia cells, myeloma cells, etc.)5
Acute GVHD (aGVHD)
All patients undergoing an allogenic stem cell transplant are at risk for developing aGVHD. Patients with one HLA mismatch (5 out of 6) are at a higher risk than those with an identical HLA match (6 out of 6). Other risk factors include patient and donor age, preparatory regimen, and the source of cells. The skin, gastrointestinal tract, and liver are the sites most often affected by aGVHD5.
- Skin aGVHD symptoms: rash: red, raised, itchy, and/or painful. Frequently begins on the hands and feet and spreads to the abdomen, chest, and upper back.
- Gastrointestinal aGVHD symptoms: diarrhea, loss of appetite, nausea, and vomiting. Can lead to gastrointestinal bleeding.
- Liver aGVHD symptoms: high levels of bilirubin, high levels of alkaline phosphate. Can lead to liver failure.
Chronic GVHD (cGVHD)
Chronic GVHD is considered an autoimmune disorder and it is the most common cause of long-term complications after transplant. A history of acute GVHD is the most important predictor of cGVHD development. Other risk factors are the same as aGVHD; patient and donor age, preparatory regimen, and source of cells. Most organ systems can be affected by cGVHD. This Long Term Survival Guidelines resource from the National Marrow Donor Program has a thorough list of symptoms of cGVHD as well as great advice on what to do after transplant.
Complications of Bone Marrow Transplant
In addition to GVHD, described above, complications may occur from the conditioning regimen and after transplant when the bone marrow is severely depleted.
Infection
Post-transplant patients are extremely vulnerable to infections (viral, bacterial, and fungal) because they lack a functional immune system2. To prevent infection patients are closely monitored, kept in protected environments, and are given a variety of prophylactic medications (medications used to prevent an illness from occurring).
Organ Effects
The conditioning regimen and the depression of the bone marrow can lead to organ problems and in some, severe cases, organ failure. Patients are closely monitored through frequent physical examinations and imaging studies. The skin, lungs, and liver are especially susceptible to the effects of the conditioning treatment2.
Gastrointestinal Tract (GI Tract) and Digestive Problems
The conditioning regimen can cause GI tract and digestive symptoms, problems may include:
- Mouth sores
- Nausea
- Vomiting
- Diarrhea
- Cramps
- Ulcers
Malnutrition
Transplant patients often have problems getting proper nutrition through food because they have a poor appetite, mouth/throat sores, and gastrointestinal issues (vomiting/diarrhea). This is usually treated with intravenous nutrition (hyperalimentation); a bag of proteins and carbohydrates that is given daily.
Bone marrow and stem cell transplantation referral line: 1-800-889-9616.
- 1abcdefg Gratwohl A. "Risk assessment in haematopoietic stem cell transplantation."Best Pract Res Clin Haematol. 2007 Jun;20(2):119-24. [PUBMED]
- 2abcde Aschan J. "Risk assessment in haematopoietic stem cell transplantation: conditioning". Best Pract Res Clin Haematol. 2007 Jun;20(2):295-310. [PUBMED]
- 3 Little, M.-T., & Storb, R. (2002). History of haematopoietic stem-cell transplantation. Nature reviews. Cancer, 2(3), 231–8. http://doi.org/10.1038/nrc748 (Original work published 2002年12月) [PUBMED]
- 4abcdefghi Chaidos A, Kanfer E, Apperley JF."Risk assessment in haemotopoietic stem cell transplantation: disease and disease stage."Best Pract Res Clin Haematol. 2007 Jun;20(2):125-54. [PUBMED]
- 5abc Holler E. "Risk assessment in haematopoietic stem cell transplantation: GvHD prevention and treatment."Best Pract Res Clin Haematol. 2007 Jun;20(2):281-94. [PUBMED]
- 6ab Dickinson AM. "Risk assessment in haematopoietic stem cell transplantation: pre-transplant patient and donor factors: non-HLA genetics."Best Pract Res Clin Haematol. 2007 Jun;20(2):189-207. [PUBMED]
- 7 Jenq, R., & van den Brink, M. (2010). Allogeneic haematopoietic stem cell transplantation: individualized stem cell and immune therapy of cancer. Nature reviews. Cancer, 10(3), 213–21. http://doi.org/10.1038/nrc2804 (Original work published 2010年12月) [PUBMED]
- 8ab Petersdorf EW. "Risk assessment in haematopoietic stem cell transplantation: histocompatibility."Best Pract Res Clin Haematol. 2007 Jun;20(2):155-70. [PUBMED]
- 9 Carreras E."Risk assessment in haematopoietic stem cell transplantation: the liver as a risk factor."Best Pract Res Clin Haematol. 2007 Jun;20(2):231-46. [PUBMED]
- 10 Ljungman P."Risk assessment in haematopoietic stem cell transplantation: viral status."Best Pract Res Clin Haematol. 2007 Jun;20(2):209-17. [PUBMED]
- 11abc Urbano-Ispizua A."Risk assessment in haematopoietic stem cell transplantation: stem cell source."Best Pract Res Clin Haematol. 2007 Jun;20(2):265-80. [PUBMED]
- 12 Barker, J., & Wagner, J. (2003). Umbilical-cord blood transplantation for the treatment of cancer. Nature reviews. Cancer, 3(7), 526–32. (Original work published 2003年7月) [PUBMED]
- 13 Hambach L, Spierings E, Goulmy E. "Risk assessment in haematopoietic stem cell transplantation: minor histocompatibility antigens."Best Pract Res Clin Haematol. 2007 Jun;20(2):171-87. [PUBMED]
