The radiation therapy video above was funded by the American Cancer Society.
- What is the difference between Chemotherapy and Radiation Therapy?
- How Radiation Therapy Works
- Types of Cancer Treated
- Radiation Therapy Planning
- Types of Radiation Therapy
- External Beam Radiation Therapy (EBRT)
- Photon Beam Therapy
- Proton Beam Therapy
- How are Photon and Proton Beam Therapies different from each other?
- Brachytherapy (BT)
- External Beam Radiation Therapy (EBRT)
- Radiation Therapy Combined with Surgery
- Advantages and Disadvantages of Radiation Therapy
- Possible Side Effects of Radiation Therapy
- The Future of Radiation Therapy
- Know the Flow: Radiation Therapy
- FAQs About Radiation Therapy
What is the difference between Chemotherapy and Radiation Therapy?
Radiation therapy uses high-energy particles or high-energy waves to kill cancer cells. Cells grow and reproduce in order to create new cells and replace cells lost to damage and aging. Cancer cells reproduce faster than normal cells and lack the controls found in normal cells. The high energy particles (or waves) kill cancer cells by causing damage to their genetic information ( DNA). DNA contains the information used to control cell growth and division.1
Radiation is a localized therapy, the high energy beams are targeted directly at the cancer. Efforts are made to avoid as many healthy cells as possible. Because this therapy is focused on a specific area of the body, it is not useful in treating cancers that may have spread to other places. Radiation therapy is used to- cure or reduce early-stage cancer, prevent cancer from returning (recurrence), treat symptoms due to advanced cancer and treat cancer that has come back.1
Chemotherapy involves using drugs to treat cancer. Unlike radiation, which is used to treat cancer in a specific region of the body, chemotherapy drugs spread throughout the body. It is used to treat tumors that can’t be removed by surgery, cancers that have spread from the original tumor to other parts of the body, and when doctors don’t know if a cancer has spread or not. Like radiation therapy, chemotherapy drugs target the division and activity of cancer cells to kill them.2
Chemotherapy is used to cure cancer, reduce how much a cancer spreads, and to reduce the pain caused by some cancers. Because the drugs used in chemotherapy affect both healthy cells and cancer cells, doctors must give a specific amount of drugs (calculated for each patient) that maintains a balance between killing cancer cells and protecting healthy cells.3
How Radiation Therapy Works
Watch the full interview with Dr. Jonathon Beitler.
Radiation therapy (or radiotherapy) is an important technique for shrinking tumors. High energy waves are targeted at the cancerous cells. The waves stop certain internal functions of the cell that are involved in cell division, so the cells eventually die.4 The death of the cells causes the tumor to shrink. One problem regarding radiotherapy is that radiation is not specific to cancerous cells and may damage healthy cells as well.
The response of tumors and normal tissues to radiation depends on their growth patterns before therapy starts and during treatment.5 Radiation kills cells through interactions with DNA and other target molecules. The cells do not die immediately; cell death occurs when the cells try to divide but fail. This is called abortive mitosis. For this reason, the cell death caused by radiation damage happens more quickly in tissues containing cells that are dividing rapidly.6
Normal tissue compensates for the cells lost during radiation treatment by accelerating the division of the remaining cells. In contrast, tumor cells actually divide more slowly after radiation treatment, and the tumor may decrease in size. The degree of tumor shrinkage depends on the balance between cell production and cell death. Carcinomas are an example of a type of cancer that often has high division rates. These types of cancer tend to respond well to radiation therapy. Depending on the dose of radiation used and the individual tumor, the tumor may start to grow again after cessation of therapy, often slower than before. To prevent regrowth of the tumor radiation is often coupled with surgery and/or chemotherapy.7
Types of Cancer Treated Using Radiation Therapy
Watch the full interview with Dr. Jonathon Beitler.
Radiation therapy is used against many types of cancer. About 60% of cancer cases require radiation therapy.8 Listed are just some of the cancers that are treated with radiotherapy: prostate, skin, head and neck, throat, larynx, breast, brain, colo-rectal, lung, bone, leukemia, ovarian, and uterine.
Certain tumors respond to radiation treatment better than others. The amount of radiation and the type needed depends on each individual case, taking into account tumor size, the stage of the cancer, tumor location, health of the patient, method of radiation delivery, and total dose.5
Certain types of cancer are considered more responsive to radiation therapy. In these cancers radiation can sometimes successfully stop growth without permanently damaging the surrounding normal tissue. If these tumors can be treated early, before metastasis the cure rate is high.5
Cancers in this category:
- skin and lip
- head and neck
- breast
- cervical and endometrium
- prostate
- Hodgkin's disease and local extranodal lymphoma
- seminoma of testis and dysgerminoma of ovary
- medulloblastoma, pineal germinoma,and ependymoma
- retinoblastoma
- choroidal melanoma
Other tumors with limited response to radiation that may be curable with combined therapies include:
- Wilms tumor
- Rhabdomyosarcoma
- colorectal cancer
- soft tissue carcinoma
- embryonal carcinoma of testis
Most other malignant cancers are not considered curable with radiation because they are difficult to detect early enough and/or they have a much higher growth rate. Tumors found in especially sensitive tissue cannot be treated with the large dose of radiation necessary to kill the tumor. Also, radiation alone is not usually successful against highly metastatic tumors. In some instances, a limited number of cures are obtained following surgery, radiation, or a combination of the two.5
Planning Radiation Therapy
Radiation can be used alone or in addition with other treatments (e.g. systemic therapy, surgery) to cure or stabilize cancer. Like other therapies, the choice to use radiation to treat a particular cancer depends on a wide range of factors. These include, but are not limited to, the type of cancer, the physical state of the patient, the stage of the cancer, and the location of the tumor. With radiation therapy, 3D models are created of the tumor and the surrounding normal structures. Radiation therapy is focused on the tumor, and the normal tissues are avoided (like a magnifying glass focusing light).
Radiation therapy – rationale and planning
Radiation can harm both cancerous and normal tissues; with radiation therapy, the goal is to maximize the damage done to cancer cells and minimize the damage to normal tissues. Radiation therapy is based on the fact that fast growing cells (e.g. cancer cells) are more sensitive to radiation damage than normal tissues; moreover, cancer cells are less likely to recover from damage of radiation therapy than normal tissues. The radiotherapy technique used depends on the type, extent and location of the cancer, and the goal of treatment.
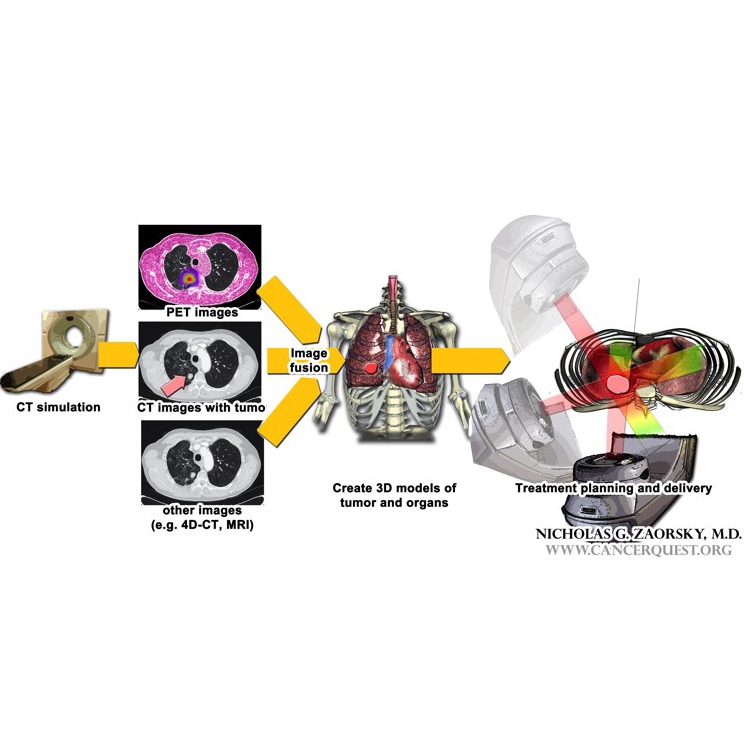
Radiation planning
In any form of radiation therapy, information from pre-treatment imaging (e.g. CT; MRI; PET-CT; 4D-CT) is combined – for external radiation, this step is called the simulation. Images are often “fused” together to give a physician detailed information about the extent of a tumor and the surrounding organs. Three dimensional models of the tumor and surrounding organs are created using a computer program. Next, a team of physicists, dosimetrists, and the physicians help create a treatment plan for the patient to maximize the delivery of radiation to the tumor and minimize the damage delivered to normal tissues.
Types of Radiation Therapy
External radiation uses machines that make high energy beams to cause damage to the genes and other parts of cancer cells.
-
External radiation uses high energy rays that are delivered to the tumor by a machine.
In internal radiation therapy, the radioactive material is placed very close to the cancer. The results is the same - cell damage and death
-
Internal radiation or brachytherapy uses a radioactive “seed” or “pellet” which is placed inside the body, in or near the tumor; the radioactive source releases energized particles that target and kill the tumor cells.
-
Systemic radiation involves introducing radioactive chemicals into the body, usually through the mouth or blood vessels (IV injection).
What is External Beam Radiation Therapy (EBRT)?
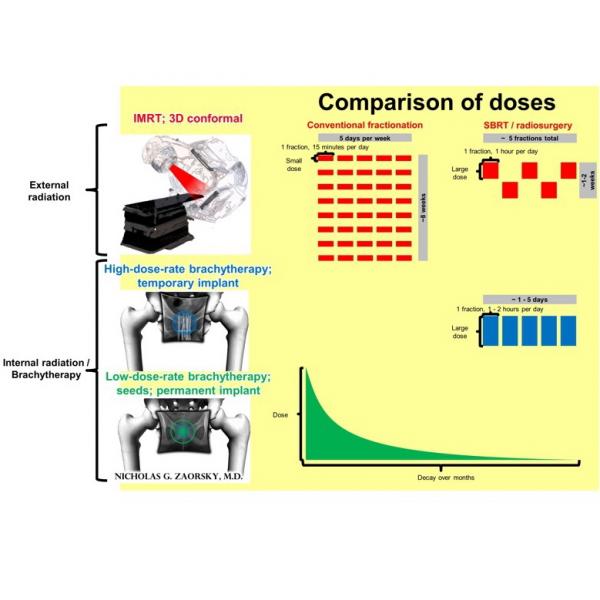
With EBRT, the patient is lying on a treatment table (black structure in the figure). An external source of radiation delivers the treatment to the volume created during planning, while minimizing the dose of radiation delivered to surrounding structures. The patient is awake during treatment; cannot feel or sense the radiation; and can resume all activities immediately following delivery of the treatment.
The common types of external radiation are: (1) intensity modulated radiation therapy (IMRT); and (2) three dimensional conformal radiation therapy (3D-CRT). IMRT is a type of EBRT that uses a multileaf collimator (MLC), a device made up of individual leaves of a high atomic numbered material that can move independently in and out of the path of a particle beam to contour its shape to a tumor, and advanced treatment planning calculation algorithms which allow for inverse optimization of MLC positioning for complex dose delivery. The dose distribution created by IMRT (vs. 3D-CRT) is characterized by less dose delivered to nearby normal tissues.
With conventional fractionation of EBRT, the patient receives single small dose, 15 minutes per day, 5 days per week, for about 2 to 8 weeks (the overall treatment time depends on the goal of therapy and other treatments involved). On the other hand, with hypofractionated techniques (e.g. stereotactic body radiation therapy [SBRT], stereotactic radiosurgery [SRS]), a large dose is delivered to the tumor in five fractions or less. The type of fractionation used depends on many factors.
What is Photon Beam Radiation Therapy?
Photon radiation uses high energy rays composed of particles of energy called photons. Photon radiation acts by disrupting the molecules of the target cells, which negatively affects the cell's functions. The common types of photon radiation are:
- Gamma rays: produced by the breakdown of radioactive isotopes of elements such as Cobalt-60 and radium
- X-rays: originate from machines that excite electrons using cathode ray tubes or linear accelerators.
These high energy particles are produced by a machine called a “linear accelerator” or “linac.” The machine is used to target photon beams at tumors inside the body.9 Photon therapy can also damage healthy cells in the body.10 Doctors who administer this therapy have to find a balance between delivering a high dose to damage the tumor, and reducing the damage of nearby healthy cells. To achieve this balance, they do the following11:
-
Target the photon beam to tumors by choosing pathways that are not too close to organs that could be damaged
-
Find several different pathways to the tumor, so that regions of healthy cells don’t get exposed to the photon beams more than necessary
-
Break down the total dose of therapy into smaller amounts delivered over time through multiple treatment sessions
A patient receiving this radiation therapy will lie down on a table with the linac moving around them to send out the photon beams from different directions. A treatment session is normally between 10 min to 30 min long. This is typically an outpatient procedure taking place 5 times per week. Because external beam radiation enters the body from the outside, normal tissues that the beams pass through can be damaged. The treatments are scheduled with this in mind, leaving enough time between sessions for damage to heal.12
What is Proton Beam Therapy?
Proton therapy is a radiation therapy that uses tiny particles called protons. Protons are excellent cell killers, but because of the way protons deliver their energy, proton therapy does not damage as much healthy tissue as much as photon therapy. Therefore, a higher dose of radiation can be targeted at the tumor without affecting many normal healthy cells.13
Protons are “sped up” or “accelerated” and released in beams by a machine called a cyclotron or a synchrotron. The initial speed of the charged particles determines how deep in the body it will travel before releasing its energy, while the strength of the beam (how powerful or energetic it is) determines the dosage of radiation delivered at the point of tumor.11
Depending on their condition, a patient receives proton therapy about 5 times a week over the course of several weeks to months. The entire session of treatment may take between 30 min to 45 min, but the actual proton therapy only takes about a minute. Radiation can not be felt, and the procedure does not cause pain. To check the effectiveness of the treatment, doctors can use imaging tools like CT scans.14
There has been limited use of particle radiotherapy, such as proton therapy, in clinical practice due to the complex and costly equipment needed for its production, but there are some advantages for using this method. It can deliver higher dose of radiation to the target volumes with less damage to the surrounding tissue. This should allow for treatment with fewer margins, more effective treatments and reduced side effects.
How are Photon and Proton Beam Therapies different from each other?
Although both photon and proton therapies are forms of radiation therapy, there are 2 main differences.
a) The type of particle that is aimed at the tumor: Photons such as X-rays are delivered as waves which do not have any charge. They pass through the body and release energy all along the way. A proton is an invisibly-small (sub-atomic) positively-charged particle. How deeply a proton travels into the body depends on the speed of the proton when it leaves the machine. 15
b) The effect of radiation on cells surrounding the tumor: The energy in photon beams ( like X-rays) gets absorbed gradually as the beams pass through tissues. Because of this, they cause damage to the tissues they pass through as they travel towards the targeted tumor. If the remaining energy of the beam is not fully absorbed by the tumor, a photon beam can continue to pass through and damage or kill more healthy cells until it exits the patient’s body.15
Protons release their energy all at once. They do not damage cells they pass through until they release their energy in a single burst. The distance that a proton travels before it releases its energy is determined by how fast it is moving. Proton beams are delivered at speeds that cause almost all of the energy to be released inside the tumor. Because all the radiation energy is targeted at the tumor, little energy is released into the tissues beyond the tumor. This saves the surrounding tissue from any damage.16
Photon therapy is often given as several weaker beams that are all focused on the target. Proton therapy is given as a single beam. Neither type of beam is visible.
What is Brachytherapy (BT)?
Brachytherapy is a radiation therapy in which the radioactive material is placed directly in or on the cancer being treated. This is done with small ‘seeds’, pellets, capsules or wire containing radioactive chemicals. Most often, the source of the radiation is inserted into the body using a needle or a catheter. Different imaging tests, including CT scans and ultrasounds are used to choose the exact position to place the radiation sources in the body. The radioactive sources release energized particles into nearby cancer cells to kill them. In brachytherapy tumors are killed from the inside. The doses of radiation used in brachytherapy are designed to target all of the cancer but to cause as little damage as possible to nearby normal tissues. Some side effects of brachytherapy are pain, swelling and bleeding at the location where the radioactive pellets are inserted.17
The types of cancer that are treated with brachytherapy include
-
Prostate
-
Cervical
-
Uterine
-
Breast
-
Lung
-
Rectal
-
Eye
-
Skin
Depending on the cancer, BT is typically given as either high-dose rate (HDR) or low-dose rate (LDR). The patient is usually under general anesthesia during any type of BT procedure. The patient can usually resume all normal activities a few days following BT.
In HDR-BT, a machine automatically releases a single small radioactive source (usually Iridium 192) through the needle inserted at specific positions delivering a high dose of radiation for a few minutes in "fractions" over the course of 1 to 10 days. The HDR-BT machine allows a physician to control the position where the radioactive source stops for a certain period of time (i.e. the “dwell position” and “dwell time,” respectively). HDR-BT is most frequently used in cancers of the prostate, cervix, uterus; it is sometimes used for cancers of the lung and breast. HDR-BT may be used alone, or it may be used as a “boost,” i.e. in addition to EBRT.
LDR-BT consists of the permanent insertion of enclosed, encapsulated sources (i.e. “seeds,” usually Iodine or Palladium), delivering a low dose of radiation that reduces over the time course of months. LDR-BT is most often used to treat prostate cancer. During the procedure, radioactive seeds (each only a few millimeters in size) are inserted directly in the tumor. The LDR-BT implantation is done once over the course of about an hour. For a man treated with LDR-BT for prostate cancer, it is typically recommended that he not have children on his lap for the first few weeks after implantation, as there may be a very small (but detectable) dose of radiation around his pelvis after the treatment during this time. LDR-BT, similar to HDR-BT, may be used alone; or it may be used as a “boost,” i.e. in addition to EBRT.
Radiation Therapy Combined with Surgery
There is ongoing discussion regarding the relative benefits of pre-operative and post-operative radiation. Both have their advantages and disadvantages. The outcome is dependent on the individual characteristics of the tumor and patient. In theory, cancer cells are growing faster before they are disturbed by surgery. At this time they should be more susceptible to radiation than in the postoperative, potentially oxygen-poor state. However, each patient's case must be assessed individually to determine the best treatment method.5
Preoperative radiation therapy:
The goal of this procedure is to kill tumor cells, shrinking the tumors and reducing the risk of metastases. Shrinking tumors with radiation may allow surgeons to remove tumors that were previously inoperable. The dosage for this procedure is usually moderate and it is used for medium-sized or advanced tumors of the head and neck, colorectum, bladder, soft-tissue sarcomas, and others.
- Advantages
- lowers risk of local recurrence and distant metastases.
- Disadvantages
- possibly obscures the extent of the tumor due to shrinkage and destruction of the margins of the tumor; this may impact the effectiveness of surgery.
- delay of surgery may cause anxiety in some patients
- increases risk of postoperative complications.
Postoperative radiation therapy:
This procedure has been shown to have the ability to eliminate any tumor cells still remaining after surgery and also reduces the occurrence of disease that may develop at the site of the surgery or in nearby lymph nodes. It is usually carried out 4-6 weeks after surgery, once the wound has healed. Postoperative radiation therapy has been shown to improve local control of head and neck, breast, gastrointestinal cancers, sarcomas etc.5
Advantages and Disadvantages of Radiation Therapy
The advantages of radiation therapy include:
- death of a large proportion of cancer cells within the entire tumor (there are minimal, if any, cancer cells are left behind in small tumors; thus, radiation alone may be used to cure certain small tumors)
- death of microscopic disease at the periphery of the tumor that would not be visible to the naked eye (e.g. at the time of surgery)
- ability to shrink tumors (which may help to relieve mass effect; or it may be done before surgery, to convert certain patients from unresectable to resectable status)
- relative safety for the patient (radiation can be delivered from outside of the body and focused on the tumor, is painless, and generally does not require anesthesia)
- synergy with systemic therapy(i.e. the ability to kill more cells together than either therapy could do alone)
- organ preservation (e.g. not removing a breast, larynx, or part of the gastrointestinal tract, which would have significant negative impact on a patient’s quality of life
- possible stimulation of an immune response against the tumor
The disadvantages of radiation therapy include:
- damage to surrounding tissues (e.g. lung, heart), depending on how close the area of interest is located to the tumor
- inability to kill tumor cells that cannot be seen on imaging scans and are therefore not always included on the 3D models (e.g. in near-by lymph nodes; metastatic disease) of radiation planning
- inability to kill the all cancer cells in tumors (this is true in particularly large tumors)
- inability to relieve mass effect (i.e. the pushing of tumor on surrounding normal structures) in certain parts of the body (e.g. brain), thereby requiring surgery
- poor killing of cancer cells in areas that do not have a good supply of oxygen (e.g. in an area after surgery; in a limb with poor blood supply)
- increased incidence in wound complication and poor healing (e.g. if surgery is used after radiation; or in parts without good circulation)
- inconvenience of radiation therapy (e.g. in some cases it must be delivered daily, 5 days per week, for 1-2 months)
- contraindications to radiation therapy (e.g. prior radiation; certain medical disorders)
Possible Side Effects of Radiation Therapy
Radiation treatments use high energy waves to damage and kill cancer cells. Because the radiation can affect cells other than cancer cells, side effects may occur. The side effects that any given patient has depends on the type and amount of radiation used and the area being treated. In general:
- The most common side effect is fatigue (in part due to energy expended in replacing normal cells killed in the process)
- The skin over the site of radiation may get red and/or sore.
- There are other side effects which are site-specific.
- Development of a second cancer, caused by the radiation therapy, is relatively uncommon, but can occur. How likely it is to happen depends on a several things, including the site being treated, and the age of the patient.
For all forms of radiation therapy:
- The treatment is painless (i.e. the patient cannot “feel” radiation)
- The patient cannot “see” the radiation (akin to getting an x-ray at the dentist)
- The patient does not “glow” or emit a light
- The patient is not radioactive (there is a small caveat with seed implantation)
- The patient cannot set off alarms in a store or an airport
- The patient will not lose hair in an untreated area (e.g. a woman being treated for breast cancer would not lose the hair on her head)
- The patient should not have nausea or vomiting, unless certain organs (e.g. esophagus, stomach, gastrointestinal tract) are treated
- Radiation therapy is not the same as uncontrolled exposure to radiation (e.g. atomic bomb, nuclear meltdown)
- The patient does not gain super powers
The Future of Radiation Therapy
Radiation therapy is an active area of research. One of the key objectives is the design of treatments that are more selective in their effects, damaging cancer cells and sparing normal cells. We will look at one current treatment being studied; Radiogenic therapy and Equivalent Uniform Dose(EUD) in conjunction with Intensity Modulated Radiation Therapy(IMRT).
Radiogenic therapy has been proposed as a method of using radiation technology to induce the formation of cytotoxic (cell killing) agents within cancer cells.18 Using lower doses of radiation with a biological agent may yield the same results as higher dose radiation alone, but with reduced toxicity. There are three groups of radiogenic therapy:
- Stimulation by radiation to directly or indirectly produce cytotoxic agents. The objective of this technique is to control genes with a radiation-inducible promoter so that they can produce cytotoxic proteins or enzymes that can then activate a drug. The activated form of the drug will kill the cancer cells.
- Auger-emitting radio-labeled molecules. These therapies can control cancer by delivering targeted radiation to specific receptor bearing cells. Auger electrons are emitted by radioactive isotopes (Iodine-125 or Indium-111). The electrons have very short ranges and therefore have the potential to be delivered to specific sets of target cells, sparing healthy cells.
- Radiation-induced genes that produce a protein that can be targeted by a cytotoxic agent.
Watch the full interview with Dr. Jonathan Beitler.
Equivalent Uniform Dose (EUD) has been proposed as an objective function of IMRT. Researchers have found that there may be just as much therapeutic benefit to administering consistent, lower-dose radiation to tumors than by varying doses dependent on the volume of the treatment field.19 Whereas IMRT varies the amount of radiation targeted at specific regions, EUD distributes equal intensities with the same efficacy, but without the same levels of toxicity.
FAQs About Radiation Therapy
RADIATION THERAPY FOR CANCER
QUESTION: What are the main treatment options for cancer? How does radiation therapy fit into these options?
ANSWER:The main treatment options for cancer are surgery, systemic therapy (for example, chemotherapy, hormones), and radiation therapy. Radiation therapy consists of either internal or external radiation. Sometimes, just one of the treatment types can be used to cure a cancer (for example, internal radiation for certain prostate cancers); other times, multiple treatment types are necessary together (for example surgery and radiation for certain breast cancers).
QUESTION: What is the goal of radiation therapy with respect to treating cancer?
ANSWER: Once a diagnosis of cancer is made, one of two goals of treatment is determined:
(1) Cure – to get rid of the cancer completely, and hopefully prevent the cancer from returning.
(2) Palliate – to make the patient’s symptoms better and improve quality of life, knowing that we likely will not cure the cancer. This applies to patients whose cancers have spread to different parts of the body.
Most patients who are treated with radiation therapy are treated for cure. You should discuss with your doctor the goal of treatment, and if it is for cure or for palliation.
QUESTION: What are the types of cancers where external radiation is used? What about internal radiation?
ANSWER: External radiation therapy is the most common type of radiation used. High energy x-rays are most commonly used to treat cancers of the lung, head & neck, prostate, breast, uterus, gastrointestinal tract (for example: rectum, pancreas, esophagus), brain, and many others. Internal radiation therapy, or an “implant,” is most commonly used for prostate cancer, gynecological cancers (specifically, endometrial or cervical cancer), and certain breast cancers.
QUESTION: Can radiation therapy alone cure me (without chemotherapy or surgery)?
ANSWER: Yes. In certain cases, radiation therapy alone can be used to cure patients. You should talk to your doctor about the treatment options that are best for you.
QUESTION: Who delivers radiation therapy? Is it a radiologist?
ANSWER: Radiation therapy is delivered in a radiation oncology department. Your doctor will be a radiation oncologist; the radiation oncologist will work with and lead a team of many others to care for you, design and deliver your treatment. For example, your treatment plan may be designed by radiation physicists and dosimetrists working with the radiation oncologist. Radiation therapists are the people who give you your daily external beam radiation treatments under the supervision of the radiation oncologist. Additionally, you will see nurses and other medical specialists from our team.
Radiologists are commonly confused with radiation oncologists. Radiologists are doctors who perform diagnostic imaging (like reading x-rays and MRIs); their input will be valuable in reviewing your scans, but they are not involved in your treatment design or delivery. Your radiation oncologist may also work closely with your other cancer doctors (like surgical oncologists or medical oncologists) to determine the treatment that is best for you.
QUESTION: Am I going to start radiation therapy on the same day that I meet the radiation oncologist?
ANSWER: Most likely not. If your radiation oncologist recommends radiation therapy, it would probably start within days to weeks -- we will explain more, in the coming questions. In certain cancer emergencies (for example, if the tumor is near the spinal cord, or a blood vessel that is critical), we will recommend starting radiation therapy on the same day as meeting you.
QUESTION: If I previously received radiation therapy, can I receive it again to a different part of the body? What about to the same part of the body?
ANSWER: If you previously received radiation therapy to one part of the body, you may receive it to a different part of the body. For example, a woman who had breast cancer and was treated with radiation therapy may later develop a uterine cancer and receive radiation treatments.
If a cancer comes back in the same area that was treated before, you may or may not be able to receive radiation to that same location. The body “remembers” where it received radiation, and there are limits to what the normal organs that surround the cancer can tolerate.
QUESTION: Can radiation therapy be used in children?
ANSWER: Yes.
QUESTION: Can radiation therapy cause me to develop cancer?
ANSWER: It is possible, but the risk of this is very low for most patients. We estimate the risk of a cancer forming from radiation therapy to be less than 0.2% per year. Thus, if the patient has many decades to live remaining (for example, a child), the risk builds up over time. On the other hand, for an adult, the risk is exceptionally low. If a second cancer were to develop, it would be near the region that received the treatment; so, you would not be more likely to form a brain cancer if you were treated for a prostate or breast cancer.
QUESTION: Should I be eating anything special during radiation therapy?
ANSWER: You should continue to eat a healthy diet. Sometimes, the cancer or the treatment may make eating certain types of foods difficult. Talk to your doctor for more details.
QUESTION: Should I be taking vitamins during radiation therapy? Can they affect how well the radiation works?
ANSWER: You should not take certain vitamins or supplements during radiation therapy. Take medications only as a treatment for another diagnosis, for example Vitamin D if you are deficient in Vitamin D. Otherwise, there is no reason to treat something that isn’t diagnosed. Large doses of antioxidants may make radiation work less well for certain cancers
EXTERNAL RADIATION THERAPY
QUESTION: How is external radiation therapy planned?
ANSWER:For external radiation therapy to work, we first need to do a “planning session” or a “simulation.” During this session, we use a CT scan, and possibly also an MRI or PET-CT scan, to take pictures of your anatomy. We then work with a team of experts to build 3 dimensional models based on these scans. The 3 dimensional models are created based on your cancer and the normal organs that surround or are next to the cancer (which we want to avoid). The radiation beam is generated inside of a special device called a linear accelerator, or a LINAC. Part of the LINAC will rotate around you during the treatment. Hundreds of very small x-ray beams will all converge at and around the cancer.
Your anatomy is unique, and it takes our team about 1-2 weeks to plan how to best design the treatment for your particular cancer. After we are finished the planning, you will be ready to start.
QUESTION:What does external radiation therapy feel like?
ANSWER: You cannot feel radiation. Radiation therapy is like getting a chest x-ray, but directed at the tumor. You are awake during the procedure. You don’t see anything. You don’t feel anything. Nothing is “burned” – contrary to what you may see in the movies. You will not glow after the treatment. You will not lose the hair on your head, unless the treatment is directed toward the brain. You will not be radioactive. You will not be a danger to anyone. You cannot get “radiation poisoning.” You will not set off alarms or bells in the airport.
Side effects from external radiation therapy depend upon the location of the treatment and the dose of radiation. The side effects of external radiation depend on the normal organs that are near the tumor. You should talk to your doctor about what side effects to expect after your treatment, and how you manage them.
QUESTION:How long does one treatment take?
ANSWER: One treatment (called a “fraction”) takes about 1 hour, from the time you get to our building, get set up, get your treatment, and exit the hospital. The actual treatment time is usually less than 5 minutes.
QUESTION: How do we know how long to treat you?
ANSWER: The length of treatment depends upon the total dose of radiation delivered and the dose per fraction. You can think of the total dose of external radiation like a brick wall. We know how “big” the wall has to be in order to stop the cancer cells. The next question is, “how big do we make the bricks?” For many cancers, we make the bricks very small, because this has been shown to reduce side effects while still being able to stop the cancer cells. Thus, many patients are treated once a day, five days per week, for about five to eight weeks.
In certain cancers (for example prostate, breast, lung), we have been able to make the bricks larger. Thus, some patients may be treated for just a few weeks.
QUESTION: What comes out of the radiation machine (or LINAC)?
ANSWER: With external radiation, the energy used is either x-rays or protons. The x-rays are similar to what is used in a chest x-ray or CT scan, only more powerful.
Protons are also available at certain hospitals for certain cancers (specifically, for pediatric cancers). For most adult cancers, protons are currently experimental and only used in specific situations.
QUESTION: How do you know you are hitting the tumor with external radiation?
ANSWER: Typically, we take x-ray pictures weekly or daily to help us direct the radiation. This is called image guidance. Sometimes, before starting radiation therapy for certain cancers we will refer you to another doctor to have small “seeds” or markers placed inside of the tumor that we can see on our scans when we deliver the treatment. The seeds are placed frequently for patients receiving radiation to the prostate, lung, or liver. The seeds will stay inside of you permanently. Please note that these seeds are different than the seeds that actually deliver radiation, as we will talk about in a bit.
QUESTION: Can you see the tumor dying?
ANSWER: Once you start receiving external radiation therapy, the radiation therapy is like putting money into an investment account: we don’t see anything after weeks or sometimes even months. The radiation effects occur over many months even after the treatment is complete. Thus, we cannot see tumors dying during treatment, and we don’t take any pictures to check. We will tell you what tests to get after you finish the treatment.
QUESTION: May I continue sexual activity during or after external radiation therapy? Will my partner be radioactive?
ANSWER: In general, for most cancers, you may continue sexual activity, though you should talk to your doctor for more details. Neither you nor your partner will be radioactive.
INTERNAL RADIATION THERAPY
QUESTION:OK, I think I understand external radiation therapy. How is internal radiation therapy planned?
ANSWER: Internal radiation therapy is also commonly known as “brachytherapy.” Internal radiation uses radiation sources that are implanted into a tumor. Internal radiation therapy is most commonly used for prostate cancer, gynecological cancers (specifically, endometrial or cervical cancer), and certain breast cancers.
For internal radiation therapy to work, we need to implant the radioactive source(s) inside of you, either for a few minutes (called high dose rate (HDR) brachytherapy), or permanently (called low dose rate (LDR) brachytherapy).
The first thing we do is a CAT scan, ultrasound, or MRI of the tumor to help find out how large it is.
QUESTION: Why not just use high dose rate (HDR) brachytherapy instead of low dose rate (LDR) brachytherapy? Won’t my dose be higher?
ANSWER: Similar to the brick wall analogy of external beam radiation therapy, the total dose, or the “size of the wall” is the same between HDR and LDR brachytherapy.
QUESTION: Am I awake during the radiation?
ANSWER: It depends on the type of tumor being treated. If we are treating prostate cancer, the patient is asleep. If we are treating endometrial cancer, the patient is awake. For cervical cancers, the patient may be sedated. You should speak to your doctor for more details.
QUESTION: Does internal radiation therapy also pass through my body like external radiation?
ANSWER: Remember how we said external radiation is like a flashlight? Internal radiation is like a very small candle: it is strong near the wick, but it becomes very weak the father away you move from it. We need to position dozens of tiny radioactive sources, which are like small candles, inside of or near the tumor to kill the cancer cells. Don’t worry, there is no “fire” or “burning” -- it’s similar to external radiation.
QUESTION: What is low dose rate brachytherapy?
ANSWER: Low dose rate brachytherapy is also called a “permanent seed implant” or “seed implant.” It is most commonly used for prostate cancer. These seeds are different than the ones we mentioned to help guide external radiation. These radioactive seeds are positioned in the prostate and give off their dose over many months. Think of it like a “cloud” of radiation covering the prostate. We only need to do this seed implant procedure once.
QUESTION: What is high dose rate brachytherapy?
ANSWER: High dose rate brachytherapy is called a “temporary implant.” We first position catheters inside or near the tumor. Next, a highly radioactive source travels through the catheters and delivers a dose of radiation to the tumor. We can fill the area where cancer cells are located with a radiation cloud. For the temporary implant, we need to do the procedure typically a few times. The procedures are typically one week apart.
QUESTION:What does internal radiation therapy feel like?
ANSWER:Similar to external radiation therapy, with internal radiation therapy, you don’t see anything. You don’t feel anything. You will not glow after the treatment. You will not lose the hair on your head. You will not be a danger to anyone. You will not set off alarms or bells in the airport
Side effects from internal radiation therapy may be present after weeks, months, or years. The side effects of internal radiation depend on the normal organs that are near the tumor. You should talk to your doctor about what side effects to expect after your treatment.
QUESTION: Can you see the tumor dying?
ANSWER: Just like external radiation, internal radiation is like putting money into an investment account: we don’t see anything after weeks or sometimes even months. The radiation effects occur over many months even after the treatment is complete. Thus, we cannot see tumors dying during treatment, and we don’t take any pictures at the time of the procedure to check. We will tell you what tests to get after you finish the treatment.
QUESTION: May I continue sexual activity during or after internal radiation therapy?
ANSWER: Since most internal radiation therapy is used for cancers near the pelvis (for example, prostate, uterus, and cervix), it is difficult to say when you would be ready for sexual activity. You should talk to your doctor for more details.
Note: This Q/A was created by Nicholas G Zaorsky, MD; Joshua E Meyer, MD; and Eric M Horwitz, MD from the Department of Radiation Oncology, Fox Chase Cancer Center.
Know the Flow: Radiation Therapy
- Drag the appropriate choices from the column on the right and place them in order in the boxes on the left. Note that you will only use five of the six choices to complete the game.
- When done, click on 'Check' to see how many you got correct.
- For incorrect answers, click on 'Description' to review information about the processes.
- To try again, choose 'Reset' and start over.
Please visit us on a larger screen to play this game.
- 1ab Radiation Therapy Basics. American Cancer Society. Accessed on 8/8/18 [LINK]
- 2 How is Chemotherapy Used to Treat Cancer? American Cancer Society. Accessed on 8/8/18 [LINK]
- 3 https://www.cancer.org/treatment/treatments-and-side-effects/treatment-types/chemotherapy/how-is-chemotherapy-used-to-treat-cancer.html
- 4 National Cancer Institute. Radiation Therapy to Treat Cancer. Accessed 1-7-2020 [Radiation Therapy to Treat Cancer.]
- 5abcdef Wang, C., M.D., ed. Clinical Radiation Oncology: Indications, Techniques, and Results. 2nd Edition. Wiley-Liss, Inc., 2000. 1-5.
- 6 Jonathan, E., Bernhard, E., & McKenna, W. (1999). How does radiation kill cells? Current opinion in chemical biology, 3(1), 77–83. (Original work published 1999年2月) [PUBMED]
- 7 Denekemp J. Cell Kinetics and Cancer Therapy. Charles C. Thomas Publisher: Illinois, 1982. 3-5, 67-69, 88-89.
- 8 RadiologyInfo.org. Accessed 10-5-2010 [http://www.radiologyinfo.org/en/info.cfm?pg=intro_onco]
- 9 "Photon Beam Radiation Therapy". National Cancer Institute. Accessed on 8/8/18 [LINK]
- 10 "External Beam Radiation Therapy". American Cancer Society. Accessed on 8/8/18 [LINK]
- 11ab Trikalinos TA, Terasawa T, Ip S, et al. Particle Beam Radiation Therapies for Cancer [Internet]. Rockville (MD): Agency for Healthcare Research and Quality (US); 2009 Nov. (Comparative Effectiveness Technical Briefs, No. 1.) Introduction. Accessed on 8/8/18 [LINK]
- 12 Radiation Therapy. Mayo Clinic. Accessed on 8/8/18 Accessed on [LINK]
- 13 External Beam Radiation Therapy. American Cancer Society. Accessed on 8/8/18 [LINK]
- 14 Proton Therapy. Mayo Clinic. Accessed on 8/8/18 [LINK]
- 15ab Trikalinos TA, Terasawa T, Ip S, et al. Particle Beam Radiation Therapies for Cancer [Internet]. Rockville (MD): Agency for Healthcare Research and Quality (US); 2009 Nov. (Comparative Effectiveness Technical Briefs, No. 1.) Introduction. Accessed on 8/8/18 [LINK] and An Introduction to Proton Therapy. OncoLink by UPenn Medicine. Accessed on 8/8/18 Accessed on [LINK]
- 16 An Introduction to Proton Therapy. OncoLink by UPenn Medicine. Accessed on 8/8/18 Accessed on [LINK]
- 17 What is Brachytherapy? Memorial Sloan Kettering Cancer Center. Accessed on 8/8/18 Accessed on [LINK]
- 18 Kaminski JM, Kaminski RJ, Dicker AP, Urbain JLC. "Defining a future role for radiogenic therapy." Cancer Treatment Reviews (2001). 27: 289-94. [PUBMED]
- 19 Wu Q, Mohan R, Niemeirko A, Schmidt UR. "Optimization of intensity-modulated radiotherapy plans based on the equivalent uniform dose." International Journal of Radiation Oncology: Biology and Physics (2002). 52: 224-35. [PUBMED]
