A wide variety of drugs is used to treat cancer. Many of them have side effects, some of them potentially serious and long-lasting.
One reason that cancer drugs tend to have many/severe side effects is that cancer cells are not very different from healthy cells. Because of this close similarity, drugs that kill cancer cells frequently also affect normal cells. Choose a topic from the list below to learn about a particular side-effect and treatments/prevention methods for that side effect.
Additional psychosocial effects, including depression, are discussed in our section on cancer survivorship.
The National Cancer Institute has produced a concise guide to survivorship that includes suggestions for how to cope with many of the side effects listed in this section. Get the guide to post-treatment survivorship from the NCI.
- Alopecia (hair loss)
- Anemia (low red blood cells counts)
- Anorexia (Inability to eat)
- Blood Clots
- Chemotherapy Induced Tissue Damage
- Diarrhea
- Fatigue
- Fertility Problems
- Gastrostomy (G-tube)
- Hand-Foot Syndrome
- Hypercalcemia
- Infections
- Insomnia (Inability to sleep)
- Low Blood Counts
- Lymphedema
- Mastectomy and Breast Reconstruction
- Memory and Concentration Problems (Chemo Brain)
- Menopausal Symptoms
- Nausea
- Neuropathy
- Neutropenia
- Oral (Mouth) Problems
- Pain
- Peripherally Inserted Central Line Catheter (PICC)
- Sexual Problems
- Swelling
- Weight Changes/Changes In Eating Habits
- Table of Treatments for Side Effects
Alopecia

Alopecia (hair loss) is one of the side effects most commonly associated with chemotherapy. Even though the loss is not associated with any physical pain or discomfort, hair loss is often one of the most distressing symptoms for patients.1, 2, 3, 4, 5, 6
A scalp cooling method to prevent hair loss has been available since the 1970s, but has not been more commonly used until recently.3 The idea behind scalp cooling is that cooling reduces blood flow to the hair follicles and prevents chemotherapy from being delivered to that portion of the body.1 The exact procedure and cooling time varies from hospital to hospital, but generally scalp cooling is used for 30 minutes before chemotherapy and for 90 minutes after the end of the infusion.2 According to a Dutch study examining 1411 patients in the Dutch Scalp Cooling Registry, about 50% of patients were satisfied enough with the scalp cooling results to wear no head cover. The large majority of patients in the registry were women with breast cancer and the effectiveness of scalp cooling largely depended on the type of chemotherapy administered. In this study 94% of patients on docetaxel, were satisfied enough with the results of scalp cooling to not a wear head cover while only 8% of patients on the TAC chemotherapy protocol wore no head cover (TAC=docetaxel/Taxotere®, doxorubicin/Adriamycin®, cyclophosphamide).3 In another Dutch study looking at the cost effectiveness of scalp cooling, scalp cooling reduced the use of wigs or a head cover by 40%.2
The main side effects of scalp cooling reported by patients were headaches and complaints of uncomfortable cold sensations.4 Few studies have examined the long-term consequences of scalp cooling. In theory, the treatment blocks chemotherapy from reaching the covered areas. This could lead to survival of cancer cells ‘hiding’ in protected areas. In a 2005 review, skin scalp metastases were found in 9 patients out of 2500. This number is very difficult to interpret because most of the studies were not designed to examine this possible side effect.5
A 2013 review showed no increased scalp metastases in breast cancer patients who used cooling. (new ref) It is possible that cancer cells protected by the cooling process could then move to a different part of the body and begin growing.7
We are not aware of any studies that have been done to examine the effects of scalp cooling on patient survival.
It is important to understand the risks that may be involved in scalp cooling and to thoroughly discuss these possibilities with your provider before making any decision.
To avoid the negative psychological impact of losing large amounts of hair (or losing clump of hair), many patients have their hair cut shorter, frequently in stages as treatment progresses. This process allows patients to become more used to having short hair, and allows people around them to get used to seeing them with less hair. Shorter hair can also lessen the trauma of hair loss because hair lost while brushing or found on a pillow appears to be less than if the hair was long. Some patients choose to shave their heads as they get farther into chemotherapy treatment. No matter how far one chooses to go, making the choice of cutting their hair can give patients a sense of control over the process.6
Anemia
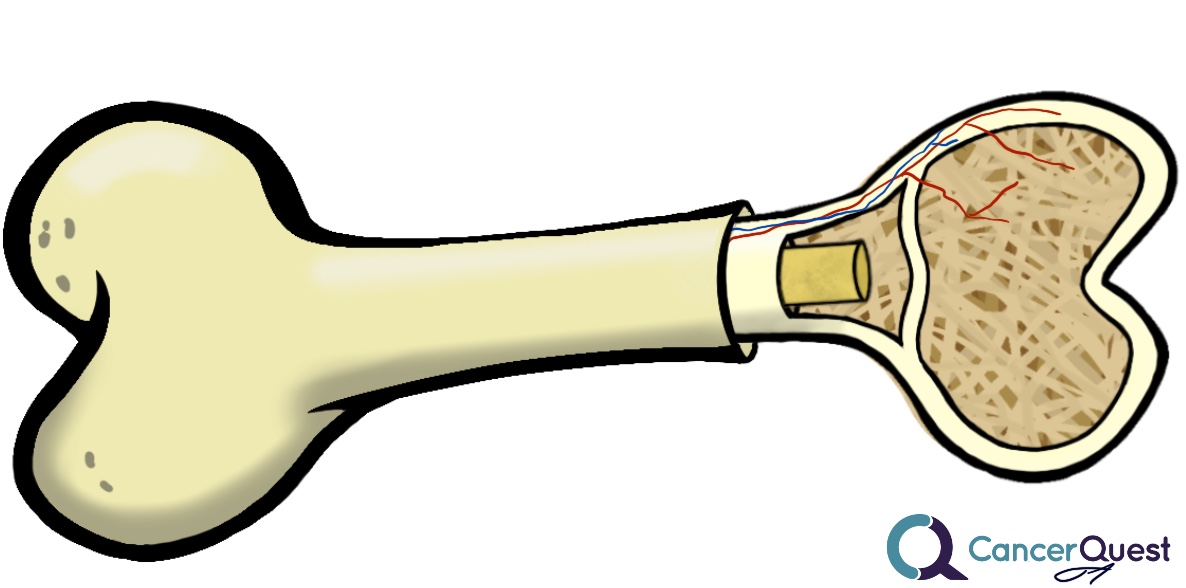
Blood cells are formed in our bones. Treatments that kill cancer cells also kill many cells in the bone marrow. This leads to a decrease in all types of blood cells, including red blood cells. Anemia is a reduction of red blood cells.
Anemia
Anemia is a reduction in the number of red blood cells circulating throughout the body. Red blood cells (also known as erythrocytes) are produced in the bone marrow and contain large amounts of the protein hemoglobin. Hemoglobin carries oxygen from the lungs to the rest of the body and helps remove carbon dioxide from the body. The NCCN recommends diagnosing anemia according to hemoglobin levels and considers a hemoglobin count of 10-11 g/dL mild anemia, 8-10 g/dL moderate anemia and less than 8 g/dL severe anemia. 8, 9
Development and Symptoms
Anemia can develop from cancer or the treatments used for cancer. It can have significant effects on treatment options, patient quality of life and patient survival. Therefore it is important to inform the doctor if any of the following symptoms are present.10
- Unusually pale skin or a hypersensitivity to cold
- Dizziness, headaches or mood changes
- Shortness of breath or labored breathing
- Rapid heartbeat or heart palpitations
- Anorexia or indigestion
- Menstrual irregularities or loss of libido
- Fatigue, including a lack of energy, weakness, difficulty concentrating, irritability, or sleep disturbances
Treatments for anemia include:
Anorexia (Inability to eat)
Anorexia, the loss of one's appetite and the desire to eat, can be caused by several different things. In cancer patients, the surgery or drugs used to treat the disease can impair eating and lower the appetite. Emotional and psychosocial factors can also induce anorexia. In some cases the patient may actually not be truly anorexic, they want to eat, but they are unable to do so. Some things that prevent cancer patients from eating include:
- Treatment with chemotherapy drugs can cause nausea, making eating difficult.
- Surgeries that can cause eating to be difficult and/or painful. Surgery to the head/neck may make eating or swallowing difficult and surgeries to the abdomen or bowels can adversely affect digestion and cause pain to occur after eating.
- Tumors themselves can interfere with the normal functioning of digestive organs (stomach, intestines, colon, pancreas), leading to loss of appetite. Tumors can also cause pain that reduces the appetite of the patient.
- The anxiety and psycho-social stress associated with a cancer diagnosis and cancer treatment can greatly impact the desire to enjoy a variety of activities, including eating.11, 12, 13, 14
The treatments for anorexia depend on the source of the problem. More than one approach might be necessary to fully address the problem. Nutritional supplements can be given to maximize the value of food that is consumed. Eating frequent small meals may also help.
Nausea associated with cancer chemotherapy can be treated with several different drugs. Learn more about treatments for nausea.
In severe cases, it might be necessary to feed an anorexic individual through a tube or intravenously. Gastrostomy tubes (G-tubes) are used to directly place food into the stomach. You can watch a documentary about gastrostomy tubes further down this page.
Blood Clots
Cancer patients are at elevated risk for developing blood clots (also called thrombosis, deep vein thrombosis or DVT). This is due to several factors including surgery, chemotherapy and effects of the cancer on the clotting system. The likelihood of developing a clot is also influenced by the individual patients' genetic make-up. The blood clots can move around the body and get stuck, cutting off the blood flow to critical organs. The movement of a blood clot is called an embolism. Embolisms can cause disability or even death so it is important to be aware of any changes in your body that may indicate the presence of a clot. Symptoms vary by the location of the blockage. As an example, blood clots that migrate to the lungs can cause shortness of breath, anxiety, pain that is often worse on inhalation, dizziness or even loss of consciousness.15, 16
Treatments exist that are able to reduce the chances that a clot will form and/or treat a clot that forms.16 Many of these drugs work by reducing unwanted clotting of the blood. Heparin is a natural protein that is used to control blood clotting. Warfarin is derived from a coumarin, a group of chemicals found in plants.17
Treatments to reduce the risk of blood clots include:
Dalteparin (Fragmin®) This is a form of heparin.
Warfarin (Coumadin®, Jantoven®, Marfarin®)
Chemotherapy Induced Tissue Damage
Many chemotherapy drugs are highly toxic. During intravenous infusion, the drug may enter the area of injection (infusion) and cause tissue damage. Drugs can get into the tissues around the injection site because of leakage around the needle or they may actually leave the blood stream after they have been injected. The process by which drugs leave a blood vessel is called extravasation. The result is that healthy tissues in the area of the injection can become irritated or even severely damaged. The actual result is dependent on the type of drug and the amount that enters the area.18
Treatments for chemotherapy induced tissue damage:
Diarrhea
Because of their effects on dividing cells, including those that line the digestive system, cancer treatments, including chemotherapy and radiation, can cause digestive problems, including diarrhea.19 Consumption of substances containing beneficial bacteria has been shown to reduce the occurrence and severity of diarrhea.20
Treatments for diarrhea include19, 21:
Fatigue
Introduction
Fatigue is a common symptom for patients with almost any cancer type 22, 23 and it can prevent normal levels of activity. About 88% of chemotherapy patients and 76% of radiation therapy patients experience fatigue. 24 It is commonly described as feeling tired, weak, exhausted, worn-out or slow. This feeling can be both acute and chronic. Acute fatigue is defined as a tired feeling that starts quickly and lasts for a short time. Chronic fatigue is a nagging weakness that is present for long periods of time.
The only way your doctors can know if you are fatigued is if you tell them, so do not be afraid to speak up. The cause of cancer related fatigue is not yet fully understood, but it is associated with the stress of the disease and its treatments. 25
Importance
Fatigue can affect cancer patients because they may not have the motivation to go to work, visit with friends, continue with treatment or continue other normal activities. A study has shown that of employed cancer patients experiencing fatigue, 75% changed their work schedule and 28% stopped working altogether. 26 Cancer related fatigue is more severe, more mentally stressful and less likely to be relieved by rest than non-cancer related fatigue. 27 Studies show that fatigue can be more distressing to patients than pain, nausea and vomiting because fatigue is not easily treated with medications. 28 Fatigue may be made worse by pain, emotional distress, eating habits, sleep patterns, decreased activity and/or other diseases. 28
Treatment
Exercise (as suggested by a doctor) and psychosocial interventions (support groups, stress management, education and behavioral intervention) often help alleviate fatigue due to chemotherapy and radiation therapy. 29, 30
Suggestions for dealing with fatigue:
- plan your events (appointments, etc.) during the times when you expect to have the most energy
- take short naps throughout the day
- let friends and family help you
- continue doing what you enjoy but monitor your energy levels and reduce the amount of time you spend doing these activities accordingly
- consider joining a support group
Watch the full interview with Jan Niles.
Fertility Problems
For patients of reproductive age, it is important that they discuss fertility issues with their oncologists. It is possible that the side effects of surgery, chemotherapy, and/or radiation may leave a patient infertile. Patients should talk with their doctors to identify options they may take before treatment to preserve their chances of having a child.31, 32, 33, 34
Sexually mature males can make deposits in a sperm bank, and prepubescent boys can have testicular tissue frozen to preserve sperm. Fertility issues are more complex for females but it is possible to extract and freeze eggs and embryos. 31, 33
For women, procedures must be specifically tailored to the patient and her needs. It is important for all female patients with the potential and desire to bear children to see a reproductive specialist before treatment begins.31, 32, 34, 35
The Oncofertility Consortium, based at Northwestern University, is dedicated to research and clinical support of cancer patients facing fertility problems.
Gastrostomy Tube (G-Tube)
Patients with head/neck cancers (i.e. tongue and throat cancer) are often treated with radiation and/or chemotherapy and surgery. The treatments may cause mouth/throat pain that makes it difficult for patients to consume enough food to maintain their health. In these cases, nutrition can be delivered via a gastrostomy tube (also called: G-tube, PEG tube or stomach tube). G-tubes may be inserted prior to treatment if it is likely that the treatments will lead to inadequate nutrition. A benefit of this preemptive insertion is that the patient does not have any throat/mouth pain that could be made worse by the insertion process. They are also healthy in terms of their nutritional status and are likely to heal quickly.
G-tubes may be inserted in several ways. Typically, they are inserted via a minimally invasive surgical procedure in which the tube is placed into the stomach via the mouth. A surgeon will then make a small incision in the abdominal wall and stomach and retrieve the tube. The tube is anchored both in the stomach and on the outside of the body. 36, 37
The videos below describe the care and maintenance of G-tubes and contain an interview with a cancer survivor who underwent the procedure.
Hand-Foot Syndrome
Some chemotherapy and targeted cancer drugs can cause painful blistering and redness of the palms of the hands and/or bottom of the feet. The affected areas may also swell up. The medical term for this is palmar-plantar erythrodysesthesia. Symptoms can include rashes, numbness, itching and tenderness (pain on contact). The symptoms occur when small amounts of the cancer drug leak out of the bloodstream and cause damage.38, 39, 40
Treatments include creams applied to the affected areas and oral pain relievers.38
Hypercalcemia
Hypercalcemia is an increase in the amount of calcium present in the blood. Calcium is an integral part of the material that makes up much of our bones (much of it stored as calcium phosphate). Release of too much calcium may lead to a wide range of symptoms including problems affecting the nervous system, kidneys and heart. The release of calcium from bones can be caused by cancer. The cancer cells responsible for the damage can be located inside or outside the affected bone(s). Cancer cells can directly damage bone or they can induce damage by activating specialized cells (osteoclasts) that break down bone.41, 42, 43
It is also possible that drugs taken to treat cancer can cause the destruction of bone. This has been documented for the anti-cancer hormonal treatment tamoxifen.44, 45
The treatments for hypercalcemia work by mechanisms that are not entirely clear. The drugs may work in several ways, two of which are shown in the animation below. The binding of the drug (pink) to the bone prevents the action of the osteoclasts. The drugs may also induce the death of the osteoclasts, reducing their number and therefore their ability to degrade the bone.41, 42, 43
Drugs used to treat hypercalcemia include:
Pamidronate disodium (Aredia)
Zoledronic acid (Zometa)
Infections
Unfortunately, chemotherapy and radiation, two common cancer treatments, can affect cells other than cancer cells. The production of white blood cells, cells of our immune system, is frequently affected. White blood cells come from cells that live in the marrow (central area) of bones. When radiation or chmotherapy damages these precursor (stem) cells, they may not be able to produce enough mature white blood cells to fight off or clear infections. Patients receiving chemotherapy and some kinds of radiation must be very careful to avoid getting an infection.
Things patients can do to help prevent infection include use of hand sanitizer, staying away from crowds of people, and wearing a protective face shield. The Centers for Disease Control and Prevention (CDC) has developed an interactive website to help patients and caregivers prevent infection. Patients can also be put on antibiotics to help prevent infection.
Patients can also receive transfusions and drugs that stimulate the bone marrow to produce more white blood cells. Because other stem cells live in the bone marrow, the treatments also affect other blood cells.
See the related side effects: Low Blood Counts, Anemia, and Neutropenia.
Insomnia (Inability to sleep)
Insomnia refers to the inability to fall asleep or to stay asleep. When insomnia lasts for 3 or more days/week, it is called insomnia syndrome. Insomnia syndrome can continue for weeks, months or longer. Because people with insomnia don’t get enough rest, they can have problems with everyday activities and suffer mental stress.
Insomnia in cancer patients can be caused by many factors including:
- The cancer cells can produce chemical signals and side effects in the body that make it difficult to fall asleep.
- Cancer treatments, including chemotherapy, can cause physical problems (nausea, diarrhea, vomiting) that make sleep difficult.
- The stress that goes along with a cancer diagnosis makes sleep difficult for many patients (and their caregivers).
- Caffeine. Eating/drinking foods that contain caffeine can cause or worsen insomnia. Foods containing caffeine include coffee, tea, chocolate, and soda.46
There are tests that doctors can use to see if a patient suffers from insomnia.
Treatments:
- There are lifestyle changes that patients with insomnia can make that can help:
- Wake up at the same time every day (regardless of how many hours of sleep one gets. This includes weekends)
- Try to get some sunlight soon after waking up. This will help your body get into a pattern of sleeping and waking up at certain times.
- Some people have difficulty falling asleep because they cannot stop thinking about problems or worries in their lives. It can help to set a daily time in the evening to think about these problems and how to solve them. This might help you get a good night’s sleep, free from worry.
- Make time to calm down 90 minutes before you plan to go to sleep. Activities such as: listening to music, reading a book, and taking a warm bath can help relax the body and mind. Too much exercise close to bedtime can make sleeping difficult.
- Only go to bed when you are feeling sleepy (regardless of what time it is) and do not spend extra time trying to sleep.
- Use your bedroom for sleep and sex only. Try not to do other daily activities on the bed (computer, phone, video games, etc.).
- If you cannot fall asleep after 20-30 minutes in bed, it is helpful to get up and do something else until you are sleepy.
- Understanding what a healthy, normal sleeping schedule is like can help get rid of worries about insomnia. It is good for normal adults to get 7-9 hours of sleep each night. As age increases, it is normal to wake up more easily during the night. However, people with insomnia are not able to fall asleep again after waking up.
- Do not take too many naps during the day. If you plan to nap, try to take your nap before 3pm. Naps later in the evening might keep you from sleeping at night.
The information above is based on - A Pan-Canadian practice guideline: prevention, screening, assessment, and treatment of sleep disturbances in adults with cancer.47
If making lifestyle changes does not help a patient fall asleep, there are medicines that can help with insomnia. These include:
Zolpidem (Ambien® -manufacturer link)
Eszopicione (Lunesta® - manufacturer link)
Ramelteon (Rozerem® - manufacturer link)
Low Blood Counts
Chemotherapy and some of other cancer treatments can have negative effects on the production of blood cells. These cells have several functions including defense against disease and carrying oxygen to all of the other cells in our bodies. When cancer treatment reduces the ability of our bodies to generate these cells, fatigue and susceptibility to disease may ensue.
The billions of blood cells that move through our circulatory system (veins, arteries, capillaries) originate from precursors that are located within our bones. These precursor cells have the ability to divide continuously. Since the majority of the cells in circulation have only short lives, the precursor (or stem) cells are able to replace those that die and are eliminated from the body.
The animation below depicts the formation of several different blood cell types from a precursor stem cell. The cells depicted (clockwise from top) include two kinds of polymorphonuclear cells (these include neutrophils), T and B lymphocytes, a megakaryocyte (makes platelets) and a red blood cell (RBC).
Many cancer treatments work by preventing the division of cells. Unfortunately, they often affect normal cells as well as cancer cells. The rapidly dividing cells within the bone marrow are often unintended targets of these drugs. The reduction in the activity of the stem cells in the bone marrow leads to two common side effects seen in cancer patients:
- Anemia: a reduction in the number of RBCs in the blood.
- Leukopenia: a reduction in the number of WBCs in the blood.
- Neutropenia: a reduction in the number of neutrophils in the blood.
- Thrombocytopenia: a reduction in the number of platelets in the blood.
Many of the blood cells affected by chemotherapy are involved in the protection of the body from disease. The drugs may weaken these defenses. Learn about the immune system.
Lymphedema
Lymphedema is a condition marked by the accumulation of fluid in the tissue surrounding capillaries. The accumulation of fluid in lymphedema is only the first stage. The following stages are a result of the buildup and may include inflammation, an increase in fatty tissue, and excess development of connective tissue. These changes can lead to an increased risk of serious infections, disfigurement, and a decrease in mobility.
The video below presents an overview of lymphedema and its treatment.
Learn more about the lymphatic system.
Overview of Lymphedema
The lymphatic system plays an important role in controlling the movement of fluid throughout the body. Specifically the lymphatic system controls the flow of lymph, a colorless fluid containing oxygen, proteins, sugar (glucose) and lymphocytes (cyte=cell). There are some similarities and differences between the (more well know) circulatory system and the lymphatic system.
Small lymphatic vessels merge into larger ones and these large vessels eventually empty into lymph nodes. Lymph nodes are kidney bean shaped tissues that are found in grape-like clusters in several locations around the body. Lymph nodes are sites of immune system activation and immune cell proliferation (growth).
Under normal conditions a clear watery fluid leaks out of the capillaries of the blood system. This fluid contains oxygen, nutrients, and other important substances needed by cells. The blood capillaries reabsorb about 90% of this fluid. The remaining 10% (lymph) is absorbed by the lymphatic system and transported back to the blood circulatory system. Normally, there is a balance of fluid leaked by the circulatory system and absorbed by the lymphatic system. This balance can be disrupted when the lymphatic system is damaged. The imbalance can lead to fluid accumulation, swelling, and eventually lymphedema.48, 49
Lymphedema is a condition marked by the accumulation of fluid in the tissue surrounding capillaries. The accumulation of fluid in lymphedema is only the first stage. The following stages are a result of the buildup and may include inflammation, an increase in fatty tissue, and excess development of connective tissue. These changes can lead to an increased risk of serious infections, disfigurement, and a decrease in mobility.48, 49
Types of Lymphedema
Primary Lymphedema
Primary lymphedema results from a condition present at birth (congenital) abnormality. This type of lymphedema is not well understood, but it is thought to be an inherited abnormality of the lymphatic system.
Secondary Lymphedema
This type of lymphedema results from disruption or destruction of a normal lymphatic system due to an injury, disease or infection, or as a side effect of a medical procedure. The most common cause worldwide is secondary to a parasitic infection. The parasite lodges itself in the lymphatic system, obstructing lymphatic vessels and disrupting lymphatic flow. In the US, however, nearly all cases are related to cancer or cancer therapy. It is frequently associated with breast cancer, prostate cancer, pelvic area cancers, lymphoma, and melanoma. Breast cancer treatment is the most common cause of cancer-related lymphedema.49, 50, 51, 52
Cancer Related Lymphedema
Because the lymphatic system is found throughout the body and carries fluid and cells, it can serve as a 'highway' for cancer cells migrating away from a tumor. When a tumor is removed, lymph nodes in the region are often removed as well, and examined for the presence of tumor cells. For many cancers, this is a routine part of the staging and treatment process. Radiation therapy used in treating cancer is often aimed at the lymph nodes in an effort to destroy any cancer cells that have drifted away from the tumor. These treatments can damage the lymphatic system resulting in the collection of lymphatic fluid in body tissues and results in swelling of the arms, legs, or trunk.49, 53, 54, 55
Stages of Lymphedema
There are four stages of lymphedema. The disease will not necessarily progress from a lower stage to a higher stage. Right now there is no cure for lymphedema, but with proper care the disease can be managed and progression can be prevented.
Stage 0 - Lymphedema is present but does not cause symptoms (subclinical). Swelling is not apparent despite reduced lymphatic function. It may exist months or years before visible swelling occurs.
Stage I - Early accumulation of fluid that is relatively high in protein content. Swelling may subside with limb elevation. Pitting of the skin may occur.
Stage II - Pitting may or may not occur as tissue fibrosis develops. Limb elevation alone rarely reduces tissue swelling.
Stage III - A severe increase in swelling may develop, along with skin changes, such as thickening of the skin, fat deposits, and warty over-growths. This stage of lymphedema may also be called lymphostatic elephantitis.
Diagnosis of Lymphedema
Early stage lymphedema is often difficult to diagnose and differentiate from other causes of swelling. In almost all cases a thorough medical history and physical examination are enough to make a diagnosis.
The following techniques may be used to rule out blood clots or other abnormalities:
Lymphoscintigraphy: uses an injection of a radioactive tracer (radiolabeled colloid) in the affected region. Imaging is done after the material has spread around the area. The resulting images provide information about the structure and function of the lymphatic system in the area.
Magnetic Resonance Imaging (MRI): MRI can provide details of the lymphatic system without the use of radiation and is highly sensitive in confirming diagnosis. The classic signs of lymphedema can be seen on MRI, including thickening of the skin, honeycombing of subcutaneous tissue, and absence of edema within the muscles.
Computed Tomography (CT): CT is used when MRI or lymphoscintigraphy is unavailable. It is highly sensitive but does not have the detailed imaging ability available with other methods.
Treatment of Lymphedema
Currently there is no cure for lymphedema. People at risk for lymphedema can try to prevent the development of the condition and for those that do have symptoms a combination of methods can be used to manage the disorder.
There are several different types of conservative treatment for lymphedema. These are treatments that do not use any kind of surgery or other invasive technique. It is important to remember that conservative techniques will only alleviate the symptoms of lymphedema and do not treat the underlying cause. Therefore, patients must continue their self care after treatment ends to obtain lasting results.
Complex Decongestive Therapy (CDT)
Complex decongestive therapy is the most common way of treating lymphedema. The basis of this treatment is to apply pressure to the affected area, squeezing the lymph fluid out of the region. This is commonly called "compression" and it is done using bandages and special clothing.
CDT is the most effective method use to treat lymphedema. It combines the use of compression techniques with manual lymphatic drainage (MLD), exercise, skin care, and self-care. When combined, these methods can significantly reduce swelling and maintain the health of the skin and supporting structures. This type of therapy benefits almost all patients when done properly, but it is time consuming, and can be expensive. It is important to find a properly trained therapist, but they are often difficult to find. Visit the Lymphology Association of North America for more information.
Pneumatic compression devices: these machines use air to squeeze the affected area in an effort to displace excess fluid. They do move fluid around, but most of the fluid is not pushed back into the lymphatic system. These machines have shown little or no long-term benefit. There are newer, more specialized pneumatic compression devices that have shown some ability to move fluid back into the lymphatic system.
Drugs and supplements: these types of treatment have shown benefits in some studies, but have shown no benefit in others. Their overall value is still under investigation.56
Surgery: surgery is not a common treatment for lymphedema. These procedures should only be used when conservative treatments have been continually unsuccessful. If surgery is suggested, patients should be well informed. As with any medical procedure, it is wise to seek a second opinion.
Surgical removal, also called debulking, is a procedure that removes excess skin and tissue. This technique does not attempt to fix lymphatic vessels or nodes. Therefore, the primary problems remain and edema may return. This type of surgery is controversial and has been shown, in some cases, to cause serious disability and permanent disfigurement.
Microsurgery attempts to correct the underlying cause of lymphedema, by transplanting lymph nodes and restructuring lymphatic vessels. This type of procedure is experimental and there is little information available about the success or side-effects of this treatment
Prevention of Lymphedema
Lymphedema can develop immediately following surgery or arise weeks, month, or even years later.57Therefore, patients at high risk should discuss preventative measures or a preventative exam with their physician. Elements of a lymphedema exam include:54, 58, 59
- Comparison of actual weight to ideal weight
- Measurements of the arms and legs
- Blood protein levels
- Assessment of ability to perform "daily activities"
- Medical illnesses including diabetes and heart disease should be considered when determining the risk of acquiring lymphedema.
If an infection occurs extra care is necessary to prevent the development of lymphedema.59, 58
Exercise after surgery (in consultation with a physician or therapist) is beneficial as it increases lymphatic drainage. For breast cancer patients, who often have lymph nodes removed from under their arms, doctors recommend exercises of hands and arms.60 Depending on the type of cancer and its involvement with local lymph nodes, physical exercises are prescribed to reduce the risk of lymphedema. A healthcare provider should be consulted to determine exercise levels that are appropriate. Some patients are afraid to exercise because they do not want to cause lymphedema. Recent work suggests that the opposite may be true; proper exercise can actually prevent lymphedema.60, 61, 62
If you notice any changes on your body, or experience any symptoms call your doctor and seek medical assistance.
Visit the NCI website for more prevention guidelines.
Frequently Asked Question: Lymphedema
If you are considered at risk for developing lymphedema, there are some things to keep in mind.
- Use care to avoid injury to the affected arm
- Use gloves for household chores
- Avoid heat; no hot baths, hot tubs, saunas
- Avoid sunburns
- Avoid tight accessories
- No blood pressure taken on affected arm
- No blood drawn or needle sticks to affected arm
- Avoid gaining excessive weight
- No lifting heavy objects (nothing more than 10-15 pounds)
- Speak to your doctor or therapist for specific recommendations
Lymphedema Resources
To Learn More Visit:
National Cancer Institute Lymphedema Page
American Cancer Society Lymphedema Page
American Cancer Society Breast Cancer & Lymphedema Page
Oncolink Gynecologic Cancer & Lymphedema Page
Oncolink Exercise & Lymphedema Page
Mastectomy and Breast Reconstruction
In general, there are two main types of breast reconstruction surgeries.
- The first type of surgery uses a saline or silicone gel-filled shell that is placed under the pectoral muscle. An expander implant is often used first in order to make room in the tissue in preparation of the final implant. The expansion greatly decreases possible implant problems.
- The second type of surgery uses skin, fat and muscle from the patient to rebuild the breast. The tissues may be obtained from several sites including the back, buttocks, thighs and abdomen.
The techniques can be used in combination on a single patient to achieve the best possible result66, 68
For a variety of reasons many women do not have breast reconstruction. These women may choose to use breast prostheses. A prosthesis is a curved form made of soft silicone that can be slipped into a special pocket on bras, clothing, and swimsuits. For women missing one breast, a prosthesis provides symmetry and balance which helps maintain good posture. Prosthetic breasts can be custom-made and are often covered by health insurance.68
Memory and Concentration Problems (Chemo Brain)
Some people who have had cancer treatment (chemotherapy or radiation to the head with high or standard dosage) experience 'brain fog' or 'chemobrain' that causes attention span and memory problems. The existence of many effects on the nervous system, including 'chemobrain' is well recognized by the medical community.71, 72
In some cases, it is unclear whether this issue is related to the treatment or the aging process. It is therefore important for survivors to speak with a doctor if they experience memory or 'thinking' problems, or if they believe that a treatment may be causing or worsening a memory or concentration problem.73, 74
Ways to improve post-treatment memory and concentration (from the NCI guide):
- write it down; bring a notepad with you to appointments
- set up reminders (e-mail, phone, text)
- group long numbers into chunks
- manage your stress
- go over what you plan to say
- repeat what you want to remember out loud
Menopausal Symptoms
Chemotherapy and other cancer treatment drugs may slow or stop a woman's menstrual cycle.75 Some cancer treatments work by reducing the amount or activity of female sex hormones leading to menopausal symptoms.76 Surgical removal of the ovaries, called oophorectomy, also results in the onset of menopause. The ovaries are a major source of the female sex hormones estrogen and progesterone.
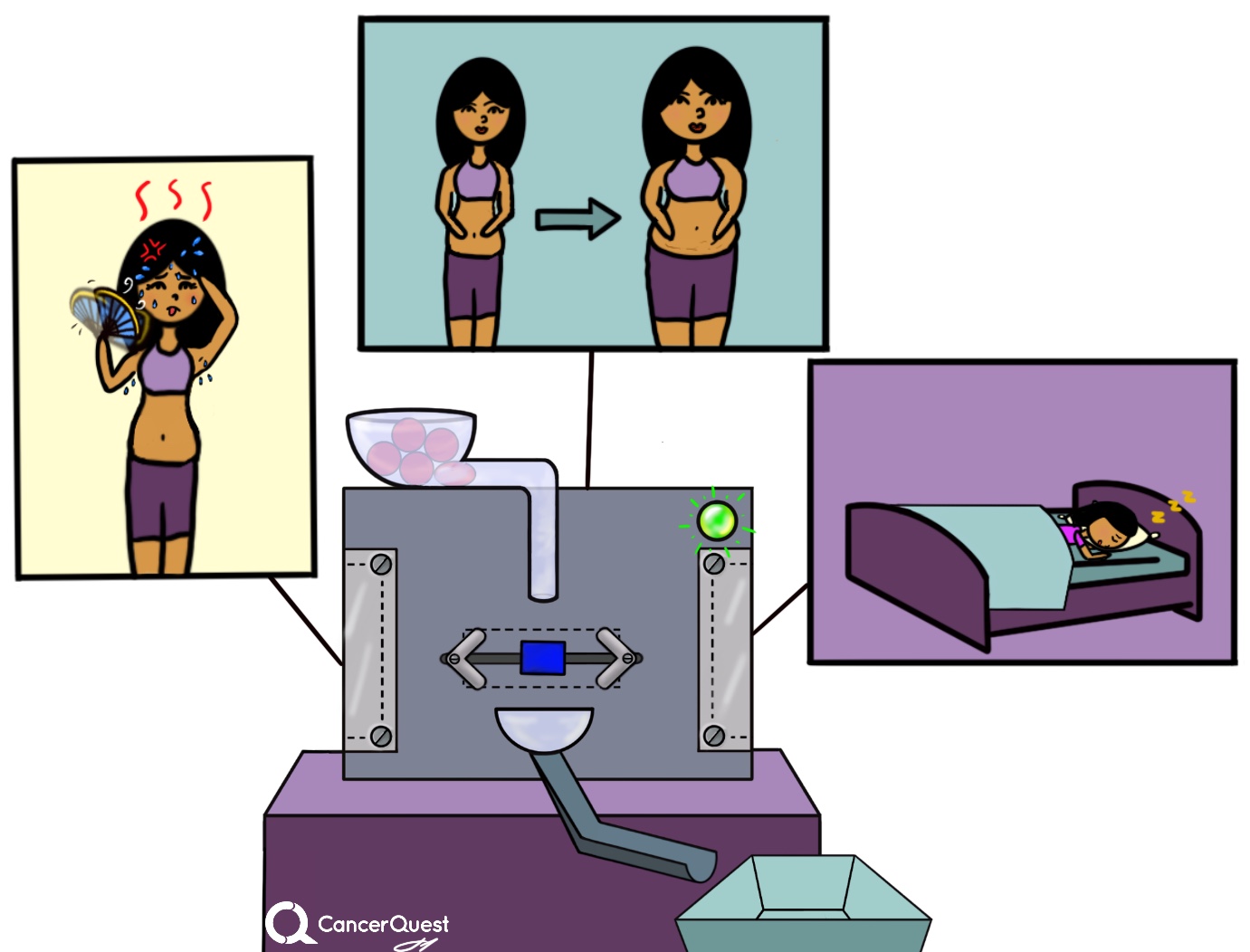
Common signs of menopause include:
- irregular periods
- hot flashes; a feeling of intense heat often accompanied by sweating
- problems with vagina and/or the bladder: tissues in these areas may experience drying and thinning which makes them prone to infection; urinary tract infections or difficulty holding urine may result
- lack of interest in sex and other sexual problems including inadequate lubrication and painful intercourse
- fatigue and sleeping problems
- memory problems, depression, mood swings, irritability
Importantly - many of the symptoms of menopause can be treated.77, 78
Nausea
Many chemotherapy agents and other cancer treatments have negative effects on the digestive system. These can be direct effects, due to the killing of cells lining the mouth, stomach and intestines, or indirect effects of the treatments. Many people find that it is easier to prevent nausea than to treat it once it has developed. For this reason it is important that you speak with your doctor about when/how you should take medication.79, 80, 81
Drugs available to treat nausea:
- Aprepitant (Emend®)
- Dolasetron (Anzemet®)
- Granisetron (Kytril®)
- Ondansetron (Zofran®)
- Palonosetron (Aloxi®)
Neuropathy (Tingling or Burning in Hands and Feet)
Chemotherapy drugs can have a variety of side effects, including damage to the nervous system. Peripheral neuropathy is damage that is felt in the hands/fingers and feet/toes. The symptoms can include pain, burning, numbness and tingling. Not all chemotherapy agents are associated with peripheral neuropathy. The likelihood of symptoms developing and their severity is dependent on the type of chemotherapy, the number of exposures (cycles/doses), the amount used, the health of the patient, the patient's genetic makeup and other factors.82 Some patients have symptoms that are severe enough to cause them to discontinue the treatment. The nerve damage and symptoms can last for many years. Patients suffering from neuropathy are more likely to have balance problems and to fall down.83
It may be possible to prevent or reduce some symptoms by putting ice packs on the hands and feet during chemotherapy infusion, but the results are not yet clear.84, 85
Neutropenia (Low White Blood Counts)
Neutropenia is an abnormally low amount of neutrophils in the blood. Neutrophils are part of the body's defense system , making up over 70% of blood leukocytes (white blood cells). Neutrophils are one of body's first lines of defense, they migrate to areas of damage/invasion and destroy foreign particles and invading microorganisms. Therefore, a patient with low levels of neutrophils is more susceptible to infection. The number of neutrophils present in the peripheral blood is reported as the absolute neutrophil count (ANC) and it is calculated in this manner:86
total leukocyte count x percentage of neutrophils and band cells = ANC
- Normal ANC - between 1500 and 7800 cells/uL
- Mild neutropenia - ANC between 1000 and 1500 cells/uL
- Moderate neutropenia - ANC between 500 and 1000 cells/uL
- Severe neutropenia - ANC below 500 cells/uL
Neutropenia can develop as a side effect of chemotherapy in as many as 40 to 80% of patients.86 It can also result from cancers of the bone marrow and metastatic solid tumors. Neutropenia can be very dangerous to the health of a cancer patient and any effort should be made to manage it effectively. One of the drugs used to stimulate the production of neutrophils is filgrastim (NEUPOGEN®).86
Filgrastim (NEUPOGEN®)
Oral (Mouth) Problems
Surgery or radiation treatment to the head and neck may cause problems with the mouth, teeth, gums, salivary glands, and/or jawbones. Some kinds of chemotherapy may cause dry mouth, cavities/other dental problems, loss of or change in sense of taste, oral infections, jaw stiffness, and jawbone changes. It is important to keep the mouth clean and moist to help limit the occurrence and/or severity of these side effects.87, 88, 89
Treatments for oral inflammation (mucositis) include several different kinds of mouthwash/rinses (sterile water, saline, sodium bicarbonate and others.) Some of the mouthwashes can contain pain medications. New agents being researched to prevent or treat mouth sores caused by cancer treatments fall into four categories: antimicrobial, coating, anti-inflammatory, and biological agents. These treatments are designed to prevent or treat the inflammation.90, 91, 92, 93
In severe cases, especially when the cancer being treated is located in the head/neck area, it may be necessary for patients to have a gastrostomy (G-tube) inserted to provide adequate nutrition.
You can learn more about gastrostomy tubes here: Gastrostomy (G-tube)
Pain
Introduction
Many cancer patients may think that pain is just a normal part of cancer/cancer treatment. They may expect pain to accompany treatment and simply "deal with it" when it arrives. Pain does not have to be an unavoidable byproduct of cancer or the treatments for cancer. There are many ways to treat cancer related pain and it can almost always be relieved. You have a right to pain relief and you should inform your doctor if you experience any discomfort. 94 If your primary doctor cannot find an appropriate plan to relieve your pain, you should seek a pain specialist. Pain is associated with tissue damage and is easiest to relieve when it is treated as early as possible. In 90% of cancer patients, pain can be controlled; unfortunately pain is often not adequately treated. 95Getting help for pain is not a sign of weakness. So be sure to tell your doctor if you feel any pain or discomfort. 96
Importance
Pain is associated with a higher level of anxiety in patients undergoing cancer treatment. 97 Unmanaged pain is also a major risk factor for depression and suicide in cancer patients. 98, 99, 100
Treatment
Treating pain makes life more enjoyable for the patient and makes completing the prescribed treatment easier. Some patients may be worried about a risk of addiction to pain medication but in actuality, only a small portion of patients become addicted to even the strongest pain killers (opioids/narcotics). 96 Nausea, sleepiness and constipation are the most common side effects that are associated with opioids. The side effects generally go away within a few days after starting treatment.
It may also be helpful for the patient to keep a diary or record of pain so the health care provider can effectively treat the pain. Generally, the goal of a successful pain management system is to decrease discomfort while increasing thinking ability, emotional well-being, and interaction with friends and family. 96
The treatments for pain described here are far from a full listing but include examples of drugs that work in a variety of ways. There are many different brands of these drugs and all brands may not be listed here for any particular drug.
Non-Steroidal Anti-Inflammatory Drugs (NSAIDs)
COX2 Inhibitors
These drugs work by inhibiting the cyclooxygenase-2 enzyme.
- Celecoxib (Celebrex®)
Opiates and derivatives
Opiates are a group of drugs containing derivatives of opium, the dried juice of a poppy seed pods. Opiates are primarily used as strong analgesics (pain relievers). Opiates also may reduce anxiety and cause drowsiness, euphoria or feelings of relaxation.
Other pain medications
Information about pain management from the American Society of Anesthesiologists (ASA).
- Opioid Treatments: https://www.asahq.org/whensecondscount/pain-management/opioid-treatment/
- Non-Opioid Treatments: https://www.asahq.org/whensecondscount/pain-management/non-opioid-treatment/
Peripherally Inserted Central Line Catheters (PICC)
Some patients have intravenous (IV) lines that remain in place for days or weeks. To avoid infection, it is important that the line(s) and the area around where the line(s) enters the body are cared for properly. The 4 videos presented here demonstrate how patients should take care of their catheters. It is also very important to notify your healthcare team if the area surrounding an IV line becomes red, painful, or swollen.
Sexual Problems
Sexual problems are very common in both male and female cancer survivors but receive little attention from clinicians.101, 102, 103, 104, 105 Many common cancer treatments, including surgery, chemotherapy, and radiation therapy, can cause physical changes that impact sexual desire and/or performance.75, 76, 106 Additionally, the stress and psychological effects of receiving a cancer diagnosis and cancer treatment can negatively influence sexual function and enjoyment. The sexual dysfunction can last for years after treatment has ended.
A major problem with sexual dysfunction is that many patients and physicians are embarrassed to bring up the topic. Research suggests that doctors do not adequately address sexual side effects of cancer/cancer treatment.107, 108 Patients may also feel that sex is not important to discuss when compared to the grave nature of the disease with which they have been diagnosed. There are treatments for many of the physical/psychological problems so it is important to talk with your physician about any concerns you may have.
The nature of some cancer types (prostate cancer, testicular cancer, cervical and other cancers of the female reproductive tract) makes their treatment more likely to negatively affect sexual function. These include:
Prostate cancer- Treatment of prostate cancer with surgery or radiation can lead to decreased ability to obtain/maintain an erection. Treatment of prostate cancer with drugs that block the activity of testosterone can also impair sexual function and/or desire. Men being treated for prostate cancer should discuss the possible effects of the treatment options on their future sexual function.106
Testicular cancer- Many survivors of testicular cancer suffer from sexual dysfunction. The symptoms range from a general lack of interest, performance problems (erection or ejaculation), and/or decreased confidence/body image problems.109, 105
Cervical cancers and other cancers of the female reproductive tract-Treatments for these cancers include surgery, radiation and chemotherapy, all of which can directly impact sexual function in women. Intercourse can be painful due to a general drying out of the vaginal canal and/or a lack of lubrication. Surgical procedures that alter the anatomy of the reproductive system may also impact sexual function/enjoyment. Treatments include vaginal moisturizers (used daily to restore normal tissues structure) and lubricants that can be used during sexual intercourse.110, 101, 102
Breast cancer- Breast cancer treatments can influence sexual function both directly and indirectly. Breast cancers can be treated with drugs that block the activity or production of the female sex hormones estrogen. These treatments can lead to symptoms similar to those found in naturally occurring menopause, including vaginal dryness.76 Even women who have gone through menopause can have their sex life impacted by the hormonal drugs used to treat cancer.78 Breast cancer survivors may also have a poor body image, leading them to feel less attractive/sexy. These concerns are frequently not addressed by medical professionals.111, 112Learn more about cancer and menopause.
Colon and rectal cancer- Both male and female survivors of colon and rectal cancer can experience sexual problems. Rectal cancer survivors were more likely to experience problems, but both sexes can be affected. Symptoms in women include vaginal dryness and pain during intercourse. Men experience erectile and ejaculation difficulties.103
Note that the list above provides only a sample of the cancers that are associated with sexual problems. Because of the wide variety of symptoms, no treatments are listed on this page. Patients and/or their partners should speak with a clinician to address any problems that occur. This is an important topic that is often overlooked so it is important to speak up!!
Swelling
Treatments for cancer (radiation and surgery) can cause patients to experience swelling of a body part due to a build-up of lymph fluid, frequently in the arms, legs, face, or neck. The swelling is called lymphedema. Cancers that are commonly associated with lymphedema include breast cancer, melanoma, cancers of the male or female reproductive organs, and cancers that have spread to the lower abdominal area.50, 51, 52
Several methods are used to treat lymphedema, including wrapping, exercises and drugs. Prevention of symptoms is important. It is important to watch for signs of swelling or infection. Symptoms to look for include redness, pain, heat, and/or fever. It is also important to protect the area of surgery or treatment and to protect the area from cuts, bug bites, and sunburn. It is important to try to avoid any trauma to the area by avoiding extreme changes in temperature, heavy lifting and excessive exercise. Recent evidence suggests that exercising the affected limb may help reduce symptoms.61, 62
Learn more and watch a documentary about lymphedema.
Learn about treatments for lymphedema.
Weight Changes/Changes In Eating Habits
Chemotherapy and other cancer treatment medications may cause patients to gain or lose weight. In the case of breast cancer, chemotherapy may cause a loss of muscle mass and an increase in fat. For some, their traditional way of losing weight (what once worked) may not work anymore. Radiation therapy or chemotherapy may also cause patients to have trouble swallowing. With time many of these problems get better. Decreased appetite and/or ability to eat can lead to malnutrition and contribute to symptoms seen in cancer patients.11, 12, 13
For those who have experienced a loss of appetite as a result of cancer treatment, there are a few key tips that can help increase food intake and reduce weight loss.
- staying active may increase a patient's appetite
- when recovering from treatment, it is best to begin by eating small meals
- stick to your favorite foods
Nutritional supplements can also help provide additional calories and nutrients. It is important to remember that supplements do NOT replace eating a balanced diet. Examples of supplements include Ensure®, BOOST® and RESOURCE®.
Also see our section on the related topic of anorexia
In severe cases, especially when the cancer being treated is located in the head/neck area, it may be necessary for patients to have a gastrostomy (G-tube) inserted to provide adequate nutrition.
Learn about gastrostomy (G-tubes or feeding tubes).
Table of Treatments for Side Effects
Treatment for Side Effects
Below is a table of drugs used to treat side effects discussed in this website. To go directly to the page where a particular drug is discussed, click on the name. For an explanation of the type of drug, click on the side effect it treats. If you have trouble finding a particular drug, go to edit on your browser and use the Find on Page feature.
More information on these drugs can be found at the FDA Approved Over the Counter and Prescription Drugs website and/or the Harrison's Principles of Internal Medicine Online. This site is only available to those with a subscription. The hardcopy version of the book is available on several online vendors
More information on this topic may be found in Chapter 16 of The Biology of Cancer by Robert A. Weinberg.
- 1ab Auvinen PK, Mähönen UA, Soininen KM, Paananen PK, Ranta-Koponen PH, Saavalainen IE, Johansson RT. The effectiveness of a scalp cooling cap in preventing chemotherapy-induced alopecia. Tumori. 2010 Mar-Apr;96(2):271-5. [PUBMED]
- 2abc van den Hurk CJ, van den Akker-van Marle ME, Breed WP, van de Poll-Franse LV, Nortier JW, Coebergh JW. Cost-effectiveness analysis of scalp cooling to reduce chemotherapy-induced alopecia. Acta Oncol. 2013 Sep 23. [Epub ahead of print] [PUBMED]
- 3abc van den Hurk CJ, Peerbooms M, van de Poll-Franse LV, Nortier JW, Coebergh JW, Breed WP. Scalp cooling for hair preservation and associated characteristics in 1411 chemotherapy patients - results of the Dutch Scalp Cooling Registry. Acta Oncol. 2012 Apr;51(4):497-504. Epub 2012 Feb 6. [PUBMED]
- 4ab Grevelman EG, Breed WP. Prevention of chemotherapy-induced hair loss by scalp cooling. Ann Oncol. 2005 Mar;16(3):352-8. Epub 2005 Jan 10. [PUBMED]
- 5ab Corina J. G. van den Hurk, Wim P. M. Breed, Floortje Mols. Chemotherapy-induced hair loss. in the Handbook of hair in health and disease. Human Health Handbooks no. 1 Volume 1, 2012, pp 402-416 [http://link.springer.com/chapter/10.3920/978-90-8686-728-8_20]
- 6ab Borsellino M, Young MM. Anticipatory coping: taking control of hair loss. Clin J Oncol Nurs. 2011 Jun;15(3):311-5. [PUBMED]
- 7 van den Hurk CJ, van de Poll-Franse LV, Breed WP, Coebergh JW, Nortier JW. Scalp cooling to prevent alopecia after chemotherapy can be considered safe in patients with breast cancer. Breast. 2013 Oct;22(5):1001-4. Epub 2013 Aug 22.
- 8 National Comprehensive Cancer Network. NCCN Clinical Practice Guidelines in Oncology: Cancer-and Treatment Related Anemia. Version 2.2010. From SABM website. Accessed January 8, 2020 [SABM Link to NCCN Anemia Guidelines]
- 9 Gilreath JA, Stenehjem DD, Rodgers GM. Diagnosis and treatment of cancer-related anemia. Am J Hematol. 2014;89(2):203–212. doi:10.1002/ajh.23628 [PubMed]
- 10 B Hurter, NJ Bush. Cancer-related anemia: clinical review and management update. Clinical Journal of Oncology Nursing. 2007 Jun;11(3):349-59. [PUBMED]
- 11ab Brown JK, Byers T, Doyle C, Coumeya KS, Demark-Wahnefried W, Kushi LH, McTieman A, Rock CL, Aziz N, Bloch AS, Eldridge B, Hamilton K, Katzin C, Koonce A, Main J, Mobley C, Morra ME, Pierce MS, Sawyer KA; American Cancer Society. Nutrition and physical activity during and after cancer treatment: an American Cancer Society guide for informed choices. CA Cancer J Clin. 2003 Sep-Oct;53(5):268-91. [PUBMED]
- 12ab van Wayenburg CA, Rasmussen-Conrad EL, van den Berg MG, Merkx MA, van Staveren WA, van Weel C, van Binsbergen JJ. Weight loss in head and neck cancer patients little noticed in general practice. J Prim Health Care. 2010 Mar;2(1):16-21. [PUBMED]
- 13ab Ströhle A, Zänker K, Hahn A. Nutrition in oncology: the case of micronutrients. Oncol Rep. 2010 Oct;24(4):815-28. [PUBMED]
- 14 Van Cutsem E, Arends J. The causes and consequences of cancer-associated malnutrition. Eur J Oncol Nurs. 2005;9 Suppl 2:S51-63. [PUBMED]
- 15 Paakauskas S., Pundzius J. and Giedrius Barauskas. Venous thromboembolism and prophylaxis in cancer patients. (2008) Medicina (Kaunas) 44(3) 175-181 [PUBMED]
- 16ab Stanley A, Young A. Primary prevention of venous thromboembolism in medical and surgical oncology patients. Br J Cancer. 2010 Apr 13;102 Suppl 1:S10-6. [PUBMED]
- 17 Hoult JR, Payá M. Pharmacological and biochemical actions of simple coumarins: natural products with therapeutic potential. Gen Pharmacol. 1996 Jun;27(4):713-22. [PUBMED]
- 18 Ener1 R. A., Meglathery1 S. B. and M. Styler. Extravasation of systemic hemato-oncological therapies. (2004) Annals of Oncology (15)858862 [PUBMED]
- 19ab Richardson G, Dobish R. Chemotherapy induced diarrhea. J Oncol Pharm Pract. 2007 Dec;13(4):181-98. [PUBMED]
- 20 Visich KL, Yeo TP. The prophylactic use of probiotics in the prevention of radiation therapy-induced diarrhea. Clin J Oncol Nurs. 2010 Aug;14(4):467-73. [PUBMED]
- 21 Benson AB 3rd, Ajani JA, Catalano RB, Engelking C, Kornblau SM, Martenson JA Jr, McCallum R, Mitchell EP, O'Dorisio TM, Vokes EE, Wadler S. Recommended guidelines for the treatment of cancer treatment-induced diarrhea. J Clin Oncol. 2004 Jul 15;22(14):2918-26. [PUBMED]
- 22 Hwang SS, Chang VT, Cogswell J, Kasimis BS. Clinical relevance of fatigue levels in cancer patients at a Veterans Administration Medical Center. Cancer 2002 94: 2481-9 [PUBMED]
- 23 Chang VT, Hwang SS, Feuerman M, Kasimis BS. Symptom and quality of life survey of medical oncology patients at a Veterans Affairs medical center: a role for symptom assessment. Cancer 2000;88:1175-83 [PUBMED]
- 24 Stasi R, Abriani L, Beccaglia P, Terzoli E, Amadori S. Cancer related fatigue: evolving concepts in evaluation and treatment. Cancer. (2003) 98: 1786-1801 [PUBMED]
- 25 The National Cancer Institute. Fatigue. U.S. National Institutes of Health. Accessed Aug. 8, 2007. [http://www.cancer.gov/cancertopics/pdq/supportivecare/fatigue/patient]
- 26 Curt GA, Breitbart W, Cella D, Groopman JE, Horning SJ, Itri LM, et al. Impact of cancer-related fatigue on the lives of patients: new findings from the Fatigue Coalition. Oncologist 2000 5:353-60. [PUBMED]
- 27 Stone P, Hardy J, Broadley K, et al. Fatigue in advanced cancer: A prospective controlled cross-sectional study. Br J Cancer 1999;79:1479-1486 [PUBMED]
- 28ab National Comprehensive Cancer Network. Cancer-related fatigue. In: Clinical Practice Guidelines in Oncology. Accessed June 20, 2006 [https://www.nccn.org/patients/resources/life_with_cancer/managing_symptoms/fatigue.aspx]
- 29 Smith GF, Toonen TR. Primary care of the patient with cancer. Am Fam Physician. 2007 Apr 15;75(8):1207-14 [PUBMED]
- 30 Uitterhoeve RJ, Vernooy M, Litjens M, Potting K, Bensing J, De Mulder P, et al. Psychosocial interventions for patients with advanced cancera systematic review of the literature. Br J Cancer 2004;91:1050-62 [PUBMED]
- 31abc Dittrich R, Maltaris T, Hoffmann I, Oppelt PG, Beckmann MW, Mueller A. Fertility preservation in cancer patients. Minerva Ginecol. 2010 Feb;62(1):63-80. [PUBMED]
- 32ab Schmidt KT, Larsen EC, Andersen CY, Andersen AN. Risk of ovarian failure and fertility preserving methods in girls and adolescents with a malignant disease. BJOG. 2010 Jan;117(2):163-74. [PUBMED]
- 33ab Mitchell RT, Saunders PT, Sharpe RM, Kelnar CJ, Wallace WH. Male fertility and strategies for fertility preservation following childhood cancer treatment. Endocr Dev. 2009;15:101-34. Epub 2009 Mar 3. [PUBMED]
- 34ab Meirow D, Nugent D. The effects of radiotherapy and chemotherapy on female reproduction. Hum Reprod Update. 2001 Nov-Dec;7(6):535-43. [PUBMED]
- 35 Georgescu ES, Goldberg JM, du Plessis SS, Agarwal A. Present and future fertility preservation strategies for female cancer patients. Obstet Gynecol Surv. 2008 Nov;63(11):725-32. [PUBMED]
- 36 Miriam Lango. "Multimodal treatment for head and neck cancer." (2009) Surgical Clin N. America 89. p43-52 [PUBMED]
- 37 Jormain Cady. "Nutritional support during radiotherapy for head and neck cancer." (2006) Clinical Journal of Oncology Nursing. 11(6) p 875-880 [PUBMED]
- 38ab Miller, K., Gorcey, L., & McLellan, B. (2014). Chemotherapy-induced hand-foot syndrome and nail changes: a review of clinical presentation, etiology, pathogenesis, and management. Journal of the American Academy of Dermatology, 71(4), 787–94. http://doi.org/10.1016/j.jaad.2014.03.019 (Original work published 2014年10月) [PUBMED]
- 39 Wilkes, G., & Doyle, D. (2005). Palmar-plantar erythrodysesthesia. Clinical journal of oncology nursing, 9(1), 103–6. (Original work published 2005年3月) [PUBMED]
- 40 Wahab, A., Khakwani, M., Ehsan, H., & Bellam, N. (2020). Paclitaxel-Induced Palmar-Plantar Erythrodysesthesia. Cureus, 12(11), e11507. http://doi.org/10.7759/cureus.11507 (Original work published 2020年11月) [PUBMED]
- 41ab Lumachi F, Brunello A, Roma A, Basso U. Cancer-induced hypercalcemia. Anticancer Res. 2009 May;29(5):1551-5. [PUBMED]
- 42ab Lumachi F, Brunello A, Roma A, Basso U. Medical treatment of malignancy-associated hypercalcemia. Curr Med Chem. 2008;15(4):415-21. [PUBMED]
- 43ab Goldner W. Cancer-Related Hypercalcemia. J Oncol Pract. 2016;12(5):426–432. doi:10.1200/JOP.2016.011155 [PubMed]
- 44 O’Connell, T. (1981). Hypercalcemia induced by tamoxifen. American journal of surgery, 141(2), 277–8. (Original work published 1981年2月) [PUBMED]
- 45 Legha, S., Powell, K., Buzdar, A., & Blumenschein, G. (1981). Tamoxifen-induced hypercalcemia in breast cancer. Cancer, 47(12), 2803–6. (Original work published 1981年6月) [PUBMED]
- 46 Heckman MA, Weil J, Gonzalez de Mejia E. Caffeine (1, 3, 7-trimethylxanthine) in foods: a comprehensive review on consumption, functionality, safety, and regulatory matters. J Food Sci. 2010 Apr;75(3):R77-87. [PUBMED]
- 47 Howell D, Oliver TK, Keller-Olaman S, Davidson J, Garland S, Samuels C, Savard J, Harris C, Aubin M, Olson K, Sussman J, Macfarlane J, Taylor C; as the Sleep Disturbance Expert Panel on behalf of the Cancer Journey Advisory Group of the Canadian Partnership Against Cancer. A Pan-Canadian practice guideline: prevention, screening, assessment, and treatment of sleep disturbances in adults with cancer. Support Care Cancer. 2013 May 25. [PUBMED]
- 48ab Wang Y, Oliver G. Current views on the function of the lymphatic vasculature in health and disease. Genes Dev. 2010 Oct 1;24(19):2115-26. [PUBMED]
- 49abcd Cormier JN, Askew RL, Mungovan KS, Xing Y, Ross MI, Armer JM. Lymphedema beyond breast cancer: a systematic review and meta-analysis of cancer-related secondary lymphedema. Cancer. 2010 Nov 15;116(22):5138-49 [PUBMED]
- 50ab Hinrichs CS, Watroba NL, Rezaishiraz H, Giese W, Hurd T, Fassl KA, Edge SB. Lymphedema secondary to postmastectomy radiation: incidence and risk factors. Ann Surg Oncol. 2004 Jun;11(6):573-80. [PUBMED]
- 51ab Fu MR, Ridner SH, Armer J. Post-breast cancer. Lymphedema: part 1. Am J Nurs. 2009 Jul;109(7):48-54; quiz 55. [PUBMED]
- 52ab Fu MR, Ridner SH, Armer J. Post-breast cancer lymphedema: part 2. Am J Nurs. 2009 Aug;109(8):34-41; quiz 42. [PUBMED]
- 53 National Lymphedema Network. What is Lymphedema Accessed January 8, 2020. [National Lymphedema Network]
- 54ab National Cancer Institute. Lymphedema. Accessed July 24, 2007 [http://www.cancer.gov/cancertopics/pdq/supportivecare/lymphedema/Patient/page2]
- 55 American Cancer Society. Understanding Lymphedema. Accessed on 8/3/2010 [http://www.cancer.org/docroot/MIT/content/MIT_7_2x_Understanding_Lymphedema.asp]
- 56 Badger C, Preston N, Seers K, Mortimer P. Benzo-pyrones for reducing and controlling lymphoedema of the limbs. Cochrane Database Syst Rev. 2004;(2):CD003140. [PUBMED]
- 57 National Lymphedema Network. A Brief Overview. Accessed July 24, 2007. [http://www.lymphnet.org/lymphedemaFAQs/overview.htm]
- 58ab Lawenda BD, Mondry TE, Johnstone PA. Lymphedema: a primer on the identification and management of a chronic condition in oncologic treatment. CA Cancer J Clin. 2009 Jan-Feb;59(1):8-24. [PUBMED]
- 59ab Bennett Britton TM, Purushotham AD. Understanding breast cancer-related lymphoedema. Surgeon. 2009 Apr;7(2):120-4. [PUBMED]
- 60ab Schmitz KH. Balancing lymphedema risk: exercise versus deconditioning for breast cancer survivors. Exerc Sport Sci Rev. 2010 Jan;38(1):17-24. [PUBMED]
- 61ab McNeely ML, Campbell K, Ospina M, Rowe BH, Dabbs K, Klassen TP, Mackey J, Courneya K. Exercise interventions for upper-limb dysfunction due to breast cancer treatment.Cochrane Database Syst Rev. 2010 Jun 16;6:CD005211. [PUBMED]
- 62ab McCausland LL. Dragon boat racing: life after breast cancer treatment. Am J Nurs. 2010 Oct;110(10):48-54. [PUBMED]
- 63abcde Morrow M, Mehrara B. "Prophylactic mastectomy and the timing of breast reconstruction." The British Journal of Surgery. 2009 Jan;96(1):1-2. [PUBMED]
- 64abc Zakaria S, Degnim AC. "Prophylactic mastectomy." Surg Clin North Am. 2007 Apr;87(2):317-31. [PUBMED]
- 65ab Spear SL, Schwarz KA, Venturi ML, Barbosa T, Al-Attar A. "Prophylactic mastectomy and reconstruction: clinical outcomes and patient satisfaction." Plast Reconstr Surg. 2008 Jul;122(1):1-9. [PUBMED]
- 66abc Cordeiro PG. "Breast reconstruction after surgery for breast cancer." N Engl J Med. 2008 Oct 9;359(15):1590-601. [PUBMED]
- 67ab N. Kropf, C. M. McCarthy, J. J. Disa."Breast Cancer Local Recurrence After Breast Reconstruction."Handchir Mikrochir Plast Chir 2008; 40: 219-224 [PUBMED]
- 68ab Hu E, Alderman AK. "Breast reconstruction." Surg Clin North Am. 2007 Apr;87(2):453-67. [PUBMED]
- 69 Ross JS, Fletcher JA, Linette GP, Stec J, Clark E, Ayers M, Symmans WF, Pusztai L, Bloom KJ. "The HER-2/neu gene and protein in breast cancer 2003: biomarker and target of therapy." The Oncologist (2003); 8:307-325 [PUBMED]
- 70ab Parker PA, Youssef A, Walker S, Basen-Engquist K, Cohen L, Gritz ER, Wei QX, Robb GL. "Short-term and long-term psychosocial adjustment and quality of life in women undergoing different surgical procedures for breast cancer." Ann Surg Oncol. 2007 Nov;14(11):3035-6. [PUBMED]
- 71 Weiss B. Evaluation of multiple neurotoxic outcomes in cancer chemotherapy. Adv Exp Med Biol. 2010;678:96-112. [PUBMED]
- 72 Weiss B. Chemobrain: a translational challenge for neurotoxicology. Neurotoxicology. 2008 Sep;29(5):891-8. Epub 2008 Apr 9. [PUBMED]
- 73 Meyers CA. "How chemotherapy damages the central nervous system." Journal of Biology (2008)7(4): 11 [http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=2397491]
- 74 CancerCare Chemobrain Information Series Cognitive Problems After Chemotherapy. [http://www.cancercare.org/pdf/fact_sheets/fs_chemobrain_cognitive.pdf]
- 75ab Torino F, Barnabei A, De Vecchis L, Appetecchia M, Strigari L, Corsello SM. Recognizing menopause in women with amenorrhea induced by cytotoxic chemotherapy for endocrine-responsive early breast cancer. Endocr Relat Cancer. 2012 Apr 10;19(2):R21-33. Print 2012 Apr. [PUBMED]
- 76abc Choueiri TK, Alemany CA, Abou-Jawde RM, Budd GT. Role of aromatase inhibitors in the treatment of breast cancer. Clin Ther. 2004 Aug;26(8):1199-214. [PUBMED]
- 77 Roush K. Managing menopausal symptoms. Am J Nurs. 2012 Jun;112(6):28-35. [PUBMED]
- 78ab Baumgart J, Nilsson K, Evers AS, Kallak TK, Poromaa IS. Sexual dysfunction in women on adjuvant endocrine therapy after breast cancer. Menopause. 2012 Sep 17. [Epub ahead of print] [PUBMED]
- 79 Jordan K, Sippel C, Schmoll HJ. Guidelines for antiemetic treatment of chemotherapy-induced nausea and vomiting: past, present, and future recommendations. Oncologist. 2007 Sep;12(9):1143-50. [PUBMED]
- 80 Frame DG.Best practice management of CINV in oncology patients: I. Physiology and treatment of CINV. Multiple neurotransmitters and receptors and the need for combination therapeutic approaches. J Support Oncol. 2010 Mar-Apr;8(2 Suppl 1):5-9. [PUBMED]
- 81 Wickham R. Best practice management of CINV in oncology patients: II. Antiemetic guidelines and rationale for use. J Support Oncol. 2010 Mar-Apr;8(2 Suppl 1):10-5. [PUBMED]
- 82 Dropcho EJ. Neurotoxicity of cancer chemotherapy. Semin Neurol. 2010 Jul;30(3):273-86. Epub 2010 Jun 24. [https://www.thieme-connect.com/DOI/DOI?10.1055/s-0030-1255217] [PUBMED]
- 83 Tofthagen C, Overcash J, Kip K. Falls in persons with chemotherapy-induced peripheral neuropathy. Support Care Cancer. 2011 Mar 5. Epub ahead of print. [PUBMED]
- 84 Ruddy, K., Le-Rademacher, J., Lacouture, M., Wilkinson, M., Onitilo, A., Woude, A., … Loprinzi, C. (2019). Randomized controlled trial of cryotherapy to prevent paclitaxel-induced peripheral neuropathy (RU221511I); an ACCRU trial. Breast (Edinburgh, Scotland), 48, 89–97. http://doi.org/10.1016/j.breast.2019.09.011 (Original work published 2019年12月) [PUBMED]
- 85 Griffiths, C., Kwon, N., Beaumont, J., & Paice, J. (2018). Cold therapy to prevent paclitaxel-induced peripheral neuropathy. Supportive care in cancer : official journal of the Multinational Association of Supportive Care in Cancer, 26(10), 3461–3469. http://doi.org/10.1007/s00520-018-4199-9 (Original work published 2018年10月) [PUBMED]
- 86abc LS Schwartzber. Neutropenia: Etiology and Pathogenesis. Clinical Cornerstone. 2006; 8 [Suppl 5]: S5-S11. [PUBMED]
- 87 Vissink A, Jansma J, Spijkervet FK, Burlage FR, Coppes RP. Oral sequelae of head and neck radiotherapy. Crit Rev Oral Biol Med. 2003;14(3):199-212. [PUBMED]
- 88 Sun HB, Gao XJ, Deng J, Li NY, Lu HJ. Progress of oral sequelae during head-neck radiotherapy. Chin J Dent Res. 2010;13(1):51-5. [PUBMED]
- 89 Djuric M, Cakic S, Hadzi-Mihailovic M, Petrovic D, Jankovic L. Oral status in patients receiving 5-fluorouracil for colorectal cancer. J BUON. 2010 Jul-Sep;15(3):475-9. [PUBMED]
- 90 Dodd MJ, Miaskowski C, Greenspan D, MacPhail L, Shih AS, Shiba G, Facione N, Paul SM. Radiation-induced mucositis: a randomized clinical trial of micronized sucralfate versus salt & soda mouthwashes. Cancer Invest. 2003;21(1):21-33. [PUBMED]
- 91 Clarkson JE, Worthington HV, Furness S, McCabe M, Khalid T, Meyer S. Interventions for treating oral mucositis for patients with cancer receiving treatment. Cochrane Database Syst Rev. 2010 Aug 4;8:CD001973. [PUBMED]
- 92 Keefe DM, Sonis ST, Bowen JM. Emerging drugs for chemotherapy-induced mucositis. Expert Opin Emerg Drugs. 2008 Sep;13(3):511-22. [PUBMED]
- 93 Worthington HV, Clarkson JE, Eden OB. Interventions for preventing oral mucositis for patients with cancer receiving treatment. Cochrane Database Syst Rev. 2007 Oct 17;(4):CD000978. [PUBMED]
- 94 Brennan F, Carr DB, Cousins M. Pain management: a fundamental human right. Anesth Analg. 2007 105(1):205-21 [PUBMED]
- 95 Weiss SC, Emanuel LL, Fairclough DL, et al.: Understanding the experience of pain in terminally ill patients. Lancet 357 (9265): 1311-5, 2001 [PUBMED]
- 96abc The National Cancer Institute. Cancer Pain. Professional Version Accessed January 8, 2020. [Cancer.gov Cancer Pain PDQ]
- 97 Stark D, Kiely M, Smith A, et al. Anxiety disorders in cancer patients: their nature, associations, and relation to quality of life. J Clin Oncol (2002) 20(14): 3137-48 [PUBMED]
- 98 Patrick DL, Ferketich SL, Frame PS, et al.: National Institutes of Health State-of-the-Science Conference Statement: Symptom Management in Cancer: Pain, Depression, and Fatigue, J Natl Cancer Inst. (2003) 95(15): 1110-7 [PUBMED]
- 99 Ciaramella A, Poli P: Assessment of depression among cancer patients: the role of pain, cancer type and treatment. Psychooncology (2001) 10 (2): 156-65 [PUBMED]
- 100 Breitbart W, Chochinov HM, Passik SD. Psychiatric symptoms in palliative medicine. In: Doyle D, Hanks G, Cherny N, Calman K (eds). The Oxford textbook of palliative medicine, 3rd edn. Oxford: Oxford University Press, 2004:74671.
- 101ab Desimone M, Spriggs E, Gass JS, Carson SA, Krychman ML, Dizon DS. Sexual Dysfunction in Female Cancer Survivors. Am J Clin Oncol. 2012 May 24. [Epub ahead of print] [PUBMED]
- 102ab Miner M, Sadovsky R, Buster JE. Hypoactive sexual desire disorder in premenopausal women: case studies. Postgrad Med. 2012 Jan;124(1):94-103. [PUBMED]
- 103ab Den Oudsten BL, Traa MJ, Thong MS, Martijn H, De Hingh IH, Bosscha K, van de Poll-Franse LV. Higher prevalence of sexual dysfunction in colon and rectal cancer survivors compared with the normative population: A population-based study. Eur J Cancer. 2012 May 16. [Epub ahead of print] [PUBMED]
- 104 Krebs, LU, 'Sexual Health During Cancer Treatment' in Reproductive Health and Cancer in Adolescents and Young Adults, Advances in Experimental Medicine and Biology 732. G.P. Quinn, S.T. Vadaparampil (eds.) Published 2012, pgs 61-76
- 105ab Kim C, McGlynn KA, McCorkle R, Li Y, Erickson RL, Ma S, Niebuhr DW, Zhang G, Zhang Y, Bai Y, Dai L, Graubard BI, Zheng T, Aschebrook-Kilfoy B, Barry KH, Zhang Y. Sexual functioning among testicular cancer survivors: A case-control study in the U.S. J Psychosom Res. 2012 Jul;73(1):68-73. Epub 2012 Apr 21. [PUBMED]
- 106ab Kyrdalen AE, Dahl AA, Hernes E, Småstuen MC, Fosså SD. A national study of adverse effects and global quality of life among candidates for curative treatment for prostate cancer. BJU Int. 2012 Jun 6. doi: 10.1111/j.1464-410X.2012.11198.x. [Epub ahead of print] [PUBMED]
- 107 Scanlon M, Blaes A, Geller M, Majhail NS, Lindgren B, Haddad T. Patient Satisfaction with Physician Discussions of Treatment Impact on Fertility, Menopause and Sexual Health among Pre-menopausal Women with Cancer. J Cancer. 2012;3:217-25. Epub 2012 May 16. [PUBMED]
- 108 Sobecki JN, Curlin FA, Rasinski KA, Lindau ST. What We Don't Talk about When We Don't Talk about Sex(1) : Results of a National Survey of U.S. Obstetrician/Gynecologists. J Sex Med. 2012 Mar 22. [Epub ahead of print] [PUBMED]
- 109 Rossen P, Pedersen AF, Zachariae R, von der Maase H. Sexuality and body image in long-term survivors of testicular cancer. Eur J Cancer. 2012 Mar;48(4):571-8. Epub 2011 Dec 23. [PUBMED]
- 110 Abbott-Anderson K, Kwekkeboom KL. A systematic review of sexual concerns reported by gynecological cancer survivors. Gynecol Oncol. 2012 Mar;124(3):477-89. Epub 2011 Nov 28. [PUBMED]
- 111 Lewis PE, Sheng M, Rhodes MM, Jackson KE, Schover LR. Psychosocial concerns of young African American breast cancer survivors. J Psychosoc Oncol. 2012 Mar;30(2):168-84. [PUBMED]
- 112 Ussher JM, Perz J, Gilbert E. Information needs associated with changes to sexual well-being after breast cancer. J Adv Nurs. 2012 Apr 15. doi: 10.1111/j.1365-2648.2012.06010.x. [Epub ahead of print] [PUBMED]
