In general, tumors can be cancerous (malignant) or non-cancerous (benign). Ovarian cancer refers to malignant tumors originating in the ovaries, which can spread (metastasize) to other places in the body. There are 3 main types of ovarian tumors. 1.
Epithelial tumors: These tumors are the most common type of ovarian tumors. These tumors originate from cells that make up the outer surface (epithelium) of the ovaries.
Germ cell tumors: These tumors originate from cells that produce eggs.
Stromal tumors: These tumors originate from cells in the ovarian stroma. Stromal cells connect the parts of the ovary together and secrete female hormones.
Ovarian cancer is the 5th leading cause of death in women. Approximately 50% of women who are diagnosed with ovarian cancer are above the age of 62. White women are more likely to get ovarian cancer than African-American women. The American Cancer Society estimates that in 2023, in the U.S., there will be approximately 19,710 new cases of ovarian cancer and approximately 13,270 women will die from ovarian cancer.2
Please visit the following sections to learn more about ovarian cancer:
- Anatomy of the ovaries
- Ovarian cancer risk factors
- Ovarian cancer prevention or protective factors
- Ovarian cancer symptoms
- Ovarian cancer detection and diagnosis
- Ovarian cancer staging
- Ovarian cancer tumor biology
- Ovarian cancer treatment
- Ovarian cancer resources
- Section Summary: Ovarian Cancer
Anatomy Of The Ovaries
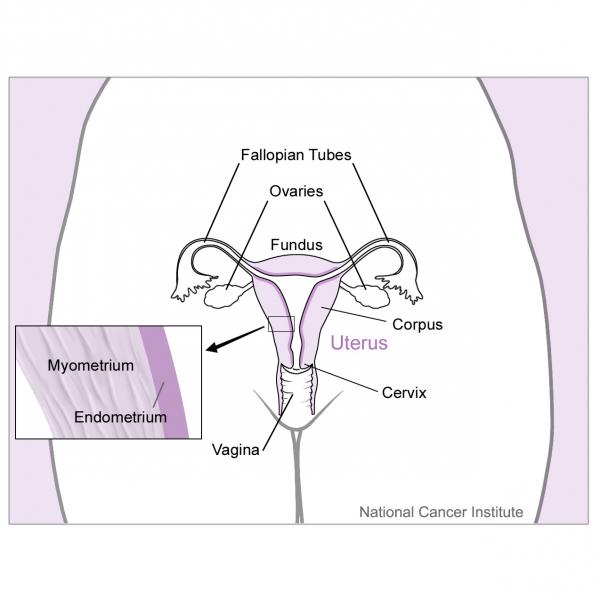
Ovaries are female reproductive organs. Women have 2 ovaries, which are located in the pelvic region, on each side of the uterus. Each ovary is approximately the size of an almond. The ovaries play a crucial role in the reproductive system. They produce and release eggs, which travel through the fallopian tubes and attach to the uterus after fertilization by a sperm. The ovaries are also responsible for producing the female sex hormones, estrogen, and progesterone3. Below is a picture of the ovaries.
The 3 main tissue types found in the ovaries are:
- Epithelial layer - this tissue type makes up the outer surface of the ovaries
- Germ layer - this tissue type is made of cells that produce eggs (ova)
- Stromal layer - this tissue type is made of cells that connect the parts of the ovary together and secrete female hormones
Also shown in the picture are:
- Uterus - the uterus is an organ located in the female pelvis. The uterus is where an unborn baby (fetus) develops inside the mother.4
- Fallopian tubes - fallopian tubes refer to the two slender tubes that allow the egg to go from the ovary to the uterus5
- Cervix - the cervix is the bottom part of the uterus that forms a passage between the uterus and vagina.6
- Myometrium - myometrium is the layer of muscleon the outside of the uterus.7
- Endometrium - endometrium is the layer of tissue that lines the uterus.8
Risk Factors
During a woman's lifetime, she has around a 1.4% chance of developing invasive ovarian cancer and around a 1.0% chance of dying from invasive ovarian cancer. The following is a list of some of the risk factors for developing ovarian cancer. Note that having a risk factor does not necessarily mean the individual will develop ovarian cancer. Furthermore, it is difficult to pinpoint exactly how big of a role a certain risk factor may have in the development of ovarian cancer10.
The following is a list of some risk factors for ovarian cancer. These risk factors are expanded upon, below.
- Family history
- Genetic predisposition
- Age
- Race
- Reproductive history
- Hormone Replacement Therapy (HRT)
- Age of first menstrual period and menopause
- Regularity and duration of menstrual cycle
- Sexual Identity
- Infertility
- Women with endometriosis
- Residence in North America
- Body-mass-index (BMI)
- Talcum powder use
Individuals with one or more family members who have or had ovarian cancer are at an increased risk for the disease. Personal or family histories of other cancers including those of the breast, uterus, colon or rectum, also increase the likelihood of ovarian cancer. Genetic counselors can help identify if individuals are at a higher risk for ovarian cancer. If there is a strong family history of ovarian cancer, genetic counseling/testing may be beneficial. Genetic counseling and testing allow the person to find out if they have genetic changes that increase their risk for getting ovarian cancer. The process includes the creation of a complete family history and performing genetic tests on a small blood sample. For someone to have a 'high-risk’ family history, the individual has to have two or more first- or second-degree relatives who have experienced ovarian cancer, early onset breast cancer (under the age of 50), bilateral breast cancer, or male breast cancers. Note that first degree relatives include a person’s mother/father/brothers/sisters and second degree relatives include grandmothers, grandfathers, grandchildren, aunts, uncles, nephews, nieces or half-siblings.11
Inherited mutations in BRCA1 and/or BRCA2 genes increase the risk of developing ovarian cancer.12
For more information about genetics screenings and tests, visit Emory University's Department of Human Genetics and Emory University's Genetics Lab.
Women over the age of 55 may be at a higher risk.11
In the U.S., African American women generally have a lower risk of developing ovarian cancer than Caucasian women do13
Older women (especially those over the age of 55) who have never been pregnant or had a child have a higher risk of ovarian cancer.13 Studies show that women who have been pregnant at least once have a decreased risk. The risk decreases further with an increasing number of pregnancies. There is a 40% reduction in risk for women who have had four or more births. Women who give birth after the age of 30-35 have a 58% decreased risk. 14.
Women who use(d) hormonal replacement therapy (HRT) to treat menopausal symptoms for 10 years or longer have an increased risk for ovarian cancer. 14.
Early age of menarche (first menstrual period) and late age of menopause are associated with increased risk. 14, 13
It has been suggested that the female homosexual population is at an increased risk of developing ovarian cancer due to a decrease in the usage of protective factors. See our page on protective factors for ovarian cancer for more information. 14
Women who are infertile may be at an increased risk of ovarian cancer. 14
Women who have endometriosis (a disorder where tissue that lines the uterus grows outside of the uterus) may be at an increased risk of ovarian cancer. 14
Residence in North America is associated with increased risk. 13
Women with short or irregular menstrual cycle lengths are at increased risk. 14
Prevention Or Protective Factors
Prevention and factors that reduce the risk for ovarian cancer include the following:
Age of first menstruation: Late-onset of menstruation (the first menstrual period is also called menarche) is associated with a lower risk of ovarian cancer 15.
Age of menopause: Early age at entering menopause is correlated with a decreased ovarian cancer risk 15.
Breastfeeding: Women who breastfed are at a decreased ovarian cancer risk 15.
Diet: No food or supplement has conclusively been shown to reduce the risk of ovarian cancer but research is ongoing. Preliminary results indicate that specific dietary items may reduce the risk of ovarian cancer. These items include:
- Vitamins A, C, D, E
- A diet that includes the recommended amount of fruits and vegetables
- Tea, especially green and black tea 15.
Hysterectomy: Women who undergo a hysterectomy (removing their ovaries) are at a decreased risk for developing ovarian cancer. However, they can still develop a rare form of cancer known as primary peritoneal carcinoma 10.
Intrauterine device (IUD): IUD use is correlated with a decrease in ovarian cancer risk 15.
Number of children: Having multiple children (multiparity) is correlated with a decreased risk for ovarian cancer 15.
Oral contraceptive use: Long-term use of oral contraceptives has been shown to reduce the risk of developing ovarian cancer. Research shows that the use of oral contraceptives reduces the risk of developing ovarian cancer in general. However, this risk reduction is maximized after 5 years of use 13. Protective benefits persist after discontinuation of OCP for at least ten, and possibly 20 years and are not dose dependent 15.
Physical activity and exercise: Healthy amounts of physical activity and exercise are associated with a lower incidence of ovarian cancer 15.
Regular health exams for women: The doctor will conduct a pelvic exam to check the size and shape of female organs. Early stage ovarian tumors may be hard to find due to its small size and location deep within the body 10.
Tubal ligation: Women who undergo tubal ligation are at a decreased risk for developing ovarian cancer 15.
Daily low dose aspirin: Preliminary research indicates that taking aspirin can help lower ovarian cancer risk and increase survival of ovarian cancer patients. Learn about ovarian cancer and aspirin on our Prevention page.
Early stages of ovarian cancer typically do not produce symptoms. Ovarian cancer that has spread (metastasized) to other parts of the body will more likely produce symptoms. The symptoms listed below may or may not be due to ovarian cancer; they may be caused by other things.10
- Abdominal swelling or bloating - this may be due to a build-up of fluid (ascites) or the presence of a tumor
- Increased pressure or pain - typically in the lower half of the body, such as the pelvis, back, abdomen or legs16
- Indigestion
- Nausea
- Constipation or diarrhea
- A feeling of fullness or inability to eat normally
- Fatigue
- Frequent urination
- Menstrual changes - this may appear as bleeding after menopause or heavy bleeding during menstruation.
- Dyspnea (shortness of breath)
- Difficulty eating16
If an individual suspects she may have ovarian cancer, she should consult a doctor who specializes in treating women with ovarian cancer. This type of doctor is known as a gynecologic oncologist. During a visit with a gynecologic oncologist, the doctor will ask the patient about her health history and may choose to conduct further tests to find out more information. The following are some examples of tests that the oncologist may perform 10. For more general information on cancer detection and diagnosis, visit CancerQuest's page: Cancer Detection and DIagnosis.
- Physical exams
During physical exams, doctors will feel (palpate) for growths and indications of fluid buildup (ascites) in the abdomen. Fluid may be sampled and examined for the presence of ovarian cancer cells. A pelvic exam is an example of a physical exam that can be used to identify lumps or changes in the shape and size of the ovaries and nearby organs.
- Ultrasound
An ultrasound may be used to detect ovarian cancer. A transvaginal ultrasound is a specific type of ultrasound where an instrument (transducer) is inserted into the vagina in order to obtain a more accurate and clearer view of the ovaries.
For more information, visit CancerQuest's page on ultrasounds.
- Biopsy
If the doctor is concerned about any lumps or changes in size/shape of an existing lump, a biopsy may be performed to detect cancer cells. In this procedure, tissue or fluid is removed from the pelvis or abdomen. There are two primary ways to perform a biopsy for ovarian cancer:
- Laparotomy - The surgeon cuts into the abdomen and examines the abdominal organs. The patient is usually given general anesthesia.
- Laparoscopy - The surgeon inserts a thin tube through a small cut in the abdomen. This procedure can be used to remove small benign cysts or ovarian cancer in its early stages. Furthermore, it can be used to see if the cancer has spread into other areas.
For more information, visit CancerQuest's page on biopsies.
- Blood tests
Some ovarian cancers produce proteins that can be detected in the blood. The proteins, which are indicators of cancer, are called ‘biomarkers’. There are several ovarian cancer biomarkers that are currently being researched.
- Examples of other tests that have been approved by the FDA to assist in the detection of ovarian cancer:
- ROMA - Risk of Ovarian Malignancy Algorithm (ROMA) uses serum levels of Human Epididymis protein 4 (HE4) and CA125, which are often overexpressed in ovarian cancer, to assess the risk of malignancy in patients with a confirmed pelvic mass. (9)
- OVA-1 - OVA-1 combines results from five tests (CA-125 II, prealbumin, apolipoprotein A-1, β2-microglobulin, and transferrin) to assess the likelihood of malignancy in women with an ovarian mass. (8)
For more information on the CA-125 test, visit CancerQuest's page on CA-125 test.
- CT scans
For information, visit CancerQuest's page on CT scans.
- MRI
For information, visit CancerQuest's page on MRI scans.
- PET scans
For information, visit CancerQuest's page on PET scans.
If cancer is found, additional tests may be conducted to determine the location of the cancer and the extent of the cancer's development.
Note: Ovarian cysts may develop on the external surface or within the ovaries; most cysts do NOT indicate the presence of cancer. Cysts typically decrease in size with time; if a cyst continues to grow it should be examined by a physician and possibly biopsied to rule out cancer. Patients should always alert their doctors to any abnormalities they detect and mention changes that occur over time. (7).
Staging
Staging allows doctors to figure out the degree to which the cancer has spread (metastasized) so that they will be able to assign a proper course of treatment. Staging is most often done during surgery, where a surgical oncologist takes tissue samples from targeted regions, such as the pelvis and abdomen, for analysis10.
There are 2 staging systems used for ovarian cancer. These systems categorize ovarian cancer based on the extent of the tumor.
- TNM staging - For information on TNM staging, visit CancerQuest's page on TNM staging.
- FIGO staging - For information on FIGO staging, visit National Cancer Institute's page on the FIGO staging system.
The following is a general summary of the stages of ovarian cancer.17
- Stage I – Cancer cells are found on the outer surface of one or both ovaries.
- Stage II – Cancer cells are found in one or both ovaries and have spread (metastasized) to the bladder, colon, rectum, or uterus.
- Stage III – Cancer cell are found in one or both ovaries and has spread (metastasized) to the abdominal lining or the lymph nodes.
- Stage IV – This is the most advanced stage of ovarian cancer. Cancer cells are found in one or both ovaries and has spread (metastasized) to the lung, liver, or other distant organs.
Tumor Biology
BRCA1 and BRCA2 genes
Genetic changes that may lead to cancer include mutations of key regulatory genes, changes in protein products, and changes in the amount of products produced by genes (gene expression). As these changes accumulate, cells become increasingly abnormal, resulting in cancer progression. Details on genetic changes that are associated with cancer can be found in the Mutation section.
The genes that are most frequently associated with ovarian cancer are the BRCA1 and BRCA2 genes. BRCA1 and BRCA2 mutations are also implicated in breast cancer (male and female), prostate cancer, and pancreatic cancer. Note that having a BRCA mutation does not mean an individual will definitely develop cancer. Rather, studies show that a BRCA mutation increases the risk of developing certain types of cancer.
- General information on BRCA1 and BRCA2 genes
The BRCA1 and BRCA2 genes are important tumor suppressor genes that are involved in the repair of damaged DNA. More information on cancer genes can be found in the Cancer Genes section.
BRCA mutations are responsible for 90% of hereditary ovarian cancer cases as well as 84% of hereditary breast cancer cases 18. However, the high percentages do not mean that BRCA mutations are common; the general population's risk of developing ovarian cancer is 1%-2%.
BRCA1 and BRCA2 mutations are germline mutations, which means the mutations are found in the DNA of eggs and sperms and can therefore, be passed down from parent to child. If an individual has a germline mutation in BRCA1, her risk of developing ovarian cancer increases from the general population's risk of (1%-2%) to 24%-40%. If an individual has a germline mutation in BRCA2, her risk of developing ovarian cancer increases from the general population's risk (1%-2%) to 11%-18%. Individuals who have 2 mutated copies of BRCA1 or 2 mutated copies of BRCA2 (homozygous for a BRCA1 or BRCA2 mutation) are at a higher risk of developing ovarian cancer than individuals who have 1 mutated copy of BRCA1 or 1 mutated copy of BRCA2 (heterozygous for a BRCA1 or BRCA2 mutation). Studies suggest that approximately 10% of women who have epithelial ovarian cancer have a germline mutation in either BRCA1 or BRCA2.19, 20
The penetrance (cancer risk) of germline mutations in BRCA1 and BRCA2 is still an ongoing area of research. This is because of the significant variability that exists between ovarian cancer cases; some individuals with a cancer-related germline mutation may never develop cancer or they may develop cancer at a later age compared with other individuals with that same cancer-related germline mutation.
- Genetic Testing for BRCA: Overview
Individuals may choose to be tested for BRCA mutations. By doing so, they will be informed of their risks for developing breast cancer, ovarian cancer, etc., and will be educated on preventive measures that may help them decrease their risks. Prior to any genetic testing, a patient must provide their informed consent in order for the test to be conducted. Genetic counselors, who are trained healthcare providers, will be present to help patients through the genetic testing process. The following are some of the main things genetic counselors do:
- Consult with patients to determine if a genetic test is necessary.
- Analyze and interpret the data from a genetic test to assess a patient's risk.
- Assist patients with the emotional and psychological toll that may be associated with genetic testing.
- Genetic Testing for BRCA: Stages
The BRCA testing process is typically separated into two stages.
- First stage - blood is drawn from the patient. The DNA from the white blood cells will then be analyzed in a laboratory to identify possible BRCA mutations.
- Second stage - this stage is similar to the first stage except blood is drawn from the patient's family members.21
Biomarkers
A biomarker is something that indirectly indicates the presence of a disease (or the potential for a disease). An example of a biomarker is cholesterol found in the blood. Measurements of blood cholesterol levels serve as indicators for cardiovascular health.
Ongoing studies are being conducted in the field of ovarian cancer biomarkers. The following are some examples of potential therapeutic biomarkers for ovarian cancer.
- FGF18 - The FGF18 gene encodes for the FGF18 protein, which is a growth factor involved in a variety of cellular activities. Although the exact mechanism of FGF18's role in ovarian cancer is still unknown, studies have linked FGF18 overexpression and gene amplification to approximately half of high-grade serous tumor cases. Studies suggest that increased levels of FGF18 protein may promote tumor growth via upregulation of the NF-kB pathway - one of the pathways implicated in ovarian cancer development. The upregulation of the NF-kB pathway leads to increased cytokine and chemokine signaling, which can lead to enhanced tumor growth.22
- HE4 - The HE4 gene encodes for the human epididymis protein, HE4. Studies have found that the HE4 protein is overexpressed in ovarian cancer. When testing for ovarian cancer tumors, HE4 can complement the commonly used ovarian cancer biomarker, cancer antigen 125 (CA 125), in order to increase the specificity and sensitivity of the biomarker detection technique.23, 24
The increase in interest in epigenetics has led to the discovery of a new type of biomarker: DNA methylation-based biomarkers. Epigenetic changes do not change the DNA sequence, but they affect how the genes function. DNA methylation, a type of epigenetic change, makes a region of genes stop working (inactivated). However, there are some hurdles to overcome in the study of epigenetics. Regarding DNA methylation-based biomarkers, studies are still ongoing as researchers try to figure out ways to distinguish between DNA methylations that are associated with cancer from DNA methylations that are simply associated with age. 25The following are some examples of DNA methylation-based biomarkers for epithelial ovarian cancer, the most prevalent form of ovarian cancer.26
- BRCA1 - hypermethylation of this gene's promoter is found in 10-15% of sporadic ovarian cancer cases and is linked to loss of gene expression
- HOXA9 - hypermethylation of this gene's CpG island promoter is found in many cancer types, such as ovarian cancer, bladder cancer, and neuroblastoma.
- MLH1 - methylation of this gene's promoter is partly responsible for the impairment of the mismatch repair pathway, which results in the resistance of epithelial ovarian cancer cells to platinum-based treatments, such as cisplatin.
Cancer Quest's focus is on the cancer's biology and the biology of possible treatments. Brief descriptions of some ovarian cancer treatments can be found below. For more detailed references of ovarian cancer treatments and guidelines, visit:
- How cancer treatments work: CancerQuest's section on Cancer Treatments
- Information regarding clinical trials:
Treatments for ovarian cancer include surgery, chemotherapy, and radiation.27 The paragraphs below describe several treatment options. The treatment that any particular patient receives will be determined by the patient and physician and depend on many factors.
- Local therapy
Local therapy includes surgery and surgery combined with other treatments (see below). It is used to eliminate the cancer from the pelvis. In addition, if ovarian cancer has spread outside of the pelvic area, local therapy can also be used to treat cancer in nearby regions.
Surgery is an option for many patients. There are two main types of surgery used to treat ovarian cancer:
- Laparotomy is a procedure in which an incision is made in the wall of the abdomen. If cancer is found, the fallopian tubes/ovaries (salpingo-oophorectomy), uterus (hysterectomy), adjacent lymph nodes, omentum (fatty tissue that supports the intestines), or tissue samples may be removed. Women of reproductive age with early stage cancer may be able to keep one ovary and fallopian tube in order to maintain reproductive capacity.
- Debulking is the removal of as much cancer as possible. Frequently, this surgery does not result in the removal of all cancer.
For more information, visit CancerQuest's page on surgery.
- Chemotherapy
Chemotherapy is a common treatment for ovarian cancer. Chemotherapy may be given in two main ways:
- Intraperitoneal chemotherapy: Drugs are infused directly into the abdomen/pelvis through a thin tube.
- Systemic chemotherapy: Drugs are taken orally or intravenously.
The timing and number of doses (also called cycles) depends on the patient and the drugs used.
For more information, visit CancerQuest's page on chemotherapy.
- Radiation Therapy
Radiation therapy (radiotherapy), which uses high-energy rays to kill cancer cells, is not commonly used for initial treatment of ovarian cancer. It may be used to relieve pain and other symptoms.
For more information, visit CancerQuest's page on radiation therapy.
Treatment by Stages:
Treatment for ovarian cancer by stage is contingent upon specific factors including: patient age, cancer stage and type of ovarian cancer, and general health conditions. Individual treatment options should be discussed with the physician.28
- Stage 1 Treatment
Often a complete abdominal hysterectomy, removal of the two ovaries and fallopian tubes (bilateral salpingo-oophorectomy), omentectomy, and removal of tissues in the pelvis and abdomen for biopsy is suggested for treatment. Individuals who have the cancer in only one ovary may have only the affected ovary and fallopian tube removed (unilateral salpingo-oophorectomy). If the cancer appears to be more likely to spread (high grade), there may be additional chemotherapy treatment. Cancer deemed less likely to spread (low-grade) is not treated with chemotherapy.
- Stages 2 and 3 Treatment
Treatment includes hysterectomy, bilateral salpingo-oophorectomy and debulking. Samples are taken from neighboring lymph nodes and other tissues in the pelvis and abdominal region to identify cancer that has spread. After surgery, patients may be treated with chemotherapy alone or both chemotherapy and radiotherapy.
- Stage 4 Treatment
Treatment includes surgery to remove as much of the tumor as possible followed by chemotherapy.
Treatment Side Effects
Certain side effects typical of chemotherapy, surgery and radiation therapy occur during treatment of ovarian cancer. However, it is important to note that everyone is different and patients respond differently to treatment.
For more general information, visit CancerQuest's page on cancer treatments.
- Chemotherapy side effects
Side effects of chemotherapy depend on which drugs are being taken. Side effects that are seen include a higher chance of infection, an increase in the likelihood of getting bruises and bleeding easily, fatigue, hair loss, decreased appetite, nausea, vomiting, and diarrhea. Click here to find more information regarding the side effects of chemotherapy.
For more information, visit CancerQuest's page on chemotherapy.
- Surgery side effects
Some pain is typical after surgery. The pain can be controlled with proper medication. The healing time varies from woman to woman and it may be several weeks before normal, everyday activities can be resumed.
For premenopausal women, surgical removal of the ovaries may cause symptoms of menopause, including hot flashes, vaginal dryness and night sweats.
For more information, visit CancerQuest's page on surgery.
- Radiation Therapy side effects
Side effects depend on the amount of radiation given and the part of your body that is treated. Radiation therapy may cause nausea, vomiting, diarrhea or bloody stools, and irradiated skin may become red, dry and tender. Learn more about the side effects of radiation therapy.
For more information, visit CancerQuest's page on radiation therapy.
Maintaining proper health during treatment for ovarian cancer:
Although it may be difficult to eat due to the side effects of treatment, patients should strive to maintain a healthy, nutritious diet. Exercise is also an important part of overall well-being after treatment. Activities such as walking, yoga and swimming may help to reduce fatigue and build strength. Always consult with your health care provider before implementing any food or exercise regimen.
Ovarian Cancer Resources
Risks for Ovarian Cancer
Risks: Ovarian Cancer (Mayo Clinic)
Risk Factors and Prevention (MSKCC)
Detection and Diagnosis of Ovarian Cancer
Winship Cancer Institute: Ovarian Cancer Diagnosis and Staging
What You Need To Know About: Ovarian Cancer (2007)
Center for Disease Control on Ovarian Cancer (CDC)
Ovarian Cancer Treatments
Treatment Guidelines for Patients (NCCN)
Ovarian Epithelial, Fallopian Tube, and Primary Peritoneal Cancer Treatment (NCI)
Ovarian Germ Cell Tumor Treatment (NCI)
Ovarian Low Malignant Potential Tumors Treatment (NCI)
Ovarian Cancer Survivorship
National Ovarian Cancer Coalition
Long Term Risks for Ovarian Cancer Survivors
Ovarian Cancer Treatment Side Effects
Chemotherapy Side Effects (OCRFA)
International Ovarian Cancer Resources
Ovarian Cancer Support Network UK
Ovarian Cancer (Cancer Research UK)
Ovarian Cancer Program Australia
Cancer Council Australia: Ovarian Cancer
Section Summary
Introduction
- Ovarian cancer is the 5th leading cause of death in women.
- Approximately 50% of women who are diagnosed with ovarian cancer are above the age of 62.
Types of Ovarian Cancer
- There are 3 main types of ovarian tumors: epithelial tumors, germ cell tumors, and stromal tumors.
- Epithelial tumors are the most common type of ovarian tumors and form on the surface of the ovaries.
Risk Factors
- Women who have one or more family members who have or had ovarian cancer, breast cancer, uterine cancer, colon cancer, or rectal cancer are at an increased risk of developing ovarian cancer.
- Women are genetically predisposed to ovarian cancer if they have inherited mutations in the BRCA1 and/or BRCA2 genes.
- Other risk factors include: age, body-mass-index (BMI), hormone replacement therapy (HRT) usage, and more.
Symptoms and Detection
- Early stages of ovarian cancer typically do not produce symptoms.
- Several medical tests can be used to detect or rule out ovarian cancer. Examples include: physical exams, CT scans, PET scans, and ultrasound scans, MRI scans, biopsies, and blood tests.
Staging and Pathology
- Two staging systems are used for ovarian cancer: TNM system and FIGO system.
- The T/N/M system assigns a degree of severity based on the size and location of the cancer.
- The FIGO system is another system used to stage the cancer based on tumor histology and how the cancer has spread.
Treatments
- Treatments depend on the patient's age, patient's health conditions, cancer stage, and type of ovarian cancer.
- Treatments can include local therapy, chemotherapy, and radiation therapy.
- 1 Kaku T1, Ogawa S, Kawano Y, Ohishi Y, Kobayashi H, Hirakawa T, Nakano H. Histological classification of ovarian cancer. Med Electron Microsc. 2003 Mar;36(1):9-17. [PUBMED]
- 2 American Cancer Society.Cancer Facts & Figures 2023. Atlanta: American Cancer Society. (2023). Retrieved from https://www.cancer.org/research/cancer-facts-statistics/all-cancer-facts-figures/2023-cancer-facts-figures.html
- 3 Karlsen MA, Sandhu N, Høgdall C, Christensen IJ, Nedergaard L, Lundvall L, Engelholm SA, Pedersen AT, Hartwell D, Lydolph M, Laursen IA, Høgdall EV. Evaluation of HE4, CA125, risk of ovarian malignancy algorithm (ROMA) and risk of malignancy index (RMI) as diagnostic tools of epithelial ovarian cancer in patients with a pelvic mass. Gynecol Oncol. 2012 Jul 24. [Epub ahead of print] PubMed PMID: 22835718. [PUBMED]
- 4 Uterus. National Cancer Institute. [http://www.cancer.gov/dictionary?CdrID=46645]
- 5 "Fallopian Tube Cancer". National Cancer Institute. [http://www.cancer.gov/dictionary?CdrID=755773]
- 6 Cervix. National Cancer Institute. [http://www.cancer.gov/dictionary?CdrID=46133]
- 7 Myometrium. National Cancer Institute. [http://www.cancer.gov/dictionary?CdrID=46280]
- 8 Endometrium. National Cancer Institute. [http://www.cancer.gov/dictionary?CdrID=46108]
- 9 Uterus and Nearby Organs. Wikimedia. National Cancer Institute. [http://upload.wikimedia.org/wikipedia/commons/7/78/Uterus_and_nearby_organs.jpg]
- 10abcdef Ovarian Cancer Overview 2014. American Cancer Society. [http://www.cancer.org/acs/groups/cid/documents/webcontent/003070-pdf.pdf]
- 11ab Reid, B., Permuth, J., & Sellers, T. (2017). Epidemiology of ovarian cancer: a review. Cancer Biology & Medicine, 14(1), 9–32. http://doi.org/10.20892/j.issn.2095-3941.2016.0084 (Original work published February 2017) [PUBMED]
- 12 Pavelka, J C, Li A J & Karlan B Y. "Hereditary Ovarian Cancer: Accessing Risk and Prevention Strategies." Obstretics and Gynecology Clnics of North America (2007): 34(4) 651-655. PMID: 18061862 [PUBMED]
- 13abcde Chobanian, N & Dietrich C S. "Ovarian Cancer." Surgical Clinics of North America (2008): 88(2) 285-299. [PUBMED]
- 14abcdefg Vo, Christine & Carney, Michael E. "Ovarian Cancer Hormonal and Environmental Risk Effect." Obstetrics and Gynecology Clnics of North America (2007): 34(4) 687-700 [PUBMED]
- 15abcdefghi Mironov S., Akin O., Pandit-Taskar N., Hann L E. "Ovarian Cancer." Radilogics Clinics of North America (2007): 45(1) 149-166. PMID: 17157627 [PUBMED]
- 16ab Andersen, R M et al."Combining a Symtoms Index with CA 125 to Improve Detention of Ovarian Cancer." Cancer (2008): v.113 (3) 1-6.
- 17 Prat, J., & Oncology, F. (2015). FIGO’s staging classification for cancer of the ovary, fallopian tube, and peritoneum: abridged republication. Journal of Gynecologic Oncology, 26(2), 87–9. http://doi.org/10.3802/jgo.2015.26.2.87 (Original work published April 2015) [PUBMED]
- 18 Marshall M, Solomon S. "Abstract Hereditary breast-ovarian cancer: clinical findings and medical management." Plast Surg Nurs. 2007 Jul-Sep;27(3):124-7. Review. [PUBMED]
- 19 Bolton KL, Chenevix-Trench G, Goh C, Sadetzki S, Ramus SJ, Karlan BY, Lambrechts D, Despierre E, Barrowdale D, McGuffog L, Healey S, Easton DF, Sinilnikova O, Benítez J, García MJ, Neuhausen S, Gail MH, Hartge P, Peock S, Frost D, Evans DG, Eeles R, Godwin AK, Daly MB, Kwong A, Ma ES, Lázaro C, Blanco I, Montagna M, D'Andrea E, Nicoletto MO, Johnatty SE, Kjaer SK, Jensen A, Hogdall E, Goode EL, Fridley BL, Loud JT, Greene MH, Mai PL, Chetrit A, Lubin F, Hirsh-Yechezkel G, Glendon G, Andrulis IL, Toland AE, Senter L, Gore ME, Gourley C, Michie CO, Song H, Tyrer J, Whittemore AS, McGuire V, Sieh W, Kristoffersson U, Olsson H, Borg Å, Levine DA, Steele L, Beattie MS, Chan S, Nussbaum RL, Moysich KB, Gross J, Cass I, Walsh C, Li AJ, Leuchter R, Gordon O, Garcia-Closas M, Gayther SA, Chanock SJ, Antoniou AC, Pharoah PD; EMBRACE; kConFab Investigators; Cancer Genome Atlas Research Network. Association between BRCA1 and BRCA2 mutations and survival in women with invasive epithelial ovarian ca [PUBMED]
- 20 Petrucelli N, Daly MB, Feldman GL. BRCA1 and BRCA2 Hereditary Breast and Ovarian Cancer. In: Pagon RA, Adam MP, Bird TD, Dolan CR, Fong CT, Stephens K, editors. SourceGeneReviews [Internet]. Seattle (WA): University of Washington, Seattle; 1993-2013. 1998 Sep 04 [updated 2013 Sep 26]. [PUBMED]
- 21 Mackay J, Taylor A. "Moving genetics into clinical cancer care: examples from BRCA gene testing and telemedicine." Breast. 2006 Dec;15 Suppl 2:S65-70. [PUBMED]
- 22 Wei W, Mok SC, Oliva E, Kim SH, Mohapatra G, Birrer MJ. FGF18 as a prognostic and therapeutic biomarker in ovarian cancer. J Clin Invest. 2013 Oct 1;123(10):4435-48. doi: 10.1172/JCI70625. Epub 2013 Sep 9. [PUBMED]
- 23 Simmons AR, Baggerly K, Bast RC Jr. The emerging role of HE4 in the evaluation of epithelial ovarian and endometrial carcinomas. Oncology (Williston Park). 2013 Jun;27(6):548-56. [PUBMED]
- 24 Van Gorp T, Cadron I, Despierre E, Daemen A, Leunen K, Amant F, Timmerman D, De Moor B, Vergote I. HE4 and CA125 as a diagnostic test in ovarian cancer: prospective validation of the Risk of Ovarian Malignancy Algorithm. Br J Cancer. 2011 Mar 1;104(5):863-70. doi: 10.1038/sj.bjc.6606092. Epub 2011 Feb 8. [PUBMED]
- 25 How Kit A, Nielsen HM, Tost J. DNA methylation based biomarkers: practical considerations and applications. Biochimie. 2012 Nov;94(11):2314-37. doi: 10.1016/j.biochi.2012.07.014. Epub 2012 Jul 27. [PUBMED]
- 26 Gloss BS, Samimi G. Epigenetic biomarkers in epithelial ovarian cancer. Cancer Lett. 2014 Jan 28;342(2):257-63. doi: 10.1016/j.canlet.2011.12.036. Epub 2012 Jan 12. [PUBMED]
- 27 Chandra, A., Pius, C., Nabeel, M., Nair, M., Vishwanatha, J., Ahmad, S., & Basha, R. (2019). Ovarian cancer: Current status and strategies for improving therapeutic outcomes. Cancer Medicine, 8(16), 7018–7031. http://doi.org/10.1002/cam4.2560 (Original work published November 2019) [PUBMED]
- 28 Treatment of invasive epithelial ovarian cancers, by stage. American Cancer Society. [http://www.cancer.org/cancer/ovariancancer/detailedguide/ovarian-cancer-treating-by-stage]