What is it?
A Positron Emission Tomography (PET) scan is an imaging technique that uses radioactive molecules to create a dynamic image of internal tissues and organs. PET scans are very useful in detecting diseases like cancer because tumors will be a different color than surrounding tissue activity. This is in contrast to techniques that reveal structure but not activity, such as a CT or X-ray.
How it works
PET scans use radioactively labeled tracers (radiotracers) that are injected into the bloodstream. Radiotracers are small molecules that are designed to be very similar to compounds normally found in the body. These specially marked compounds are used in normal body processes, but emit positrons as they break down. PET scanners contain special cameras that detect these positrons and create images with the information. The image distinguishes areas that have little radiotracer concentration from areas with increased concentrations of radiotracer. On the image, the differences are represented by color changes.
Below is a list of the information included in this section:
Equipment
What instruments are used?
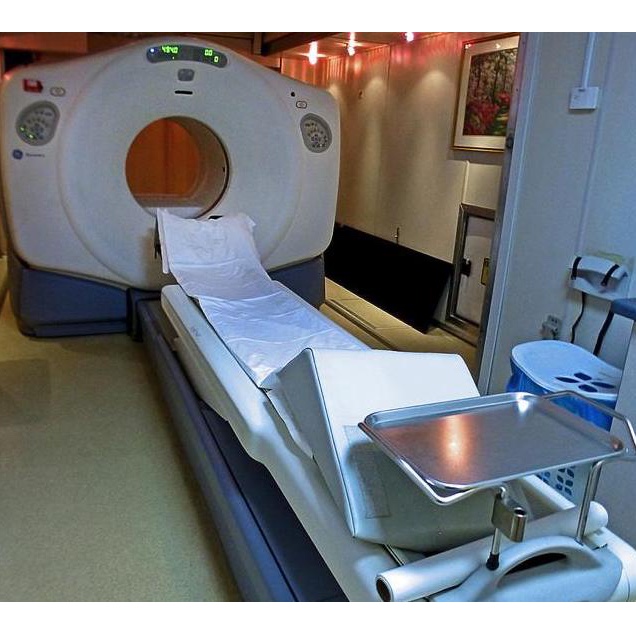
A PET scanner looks very similar to a CT scanner and in many cases it is the same machine. There are 4 main components a PET scan machine, the gantry (frame) that houses the detection apparatus with a large patient port (opening), the subject table that moves in and out of the patient port allowing for a complete scan, the detector/camera system that captures the image, and a computer system that processes and presents the images.
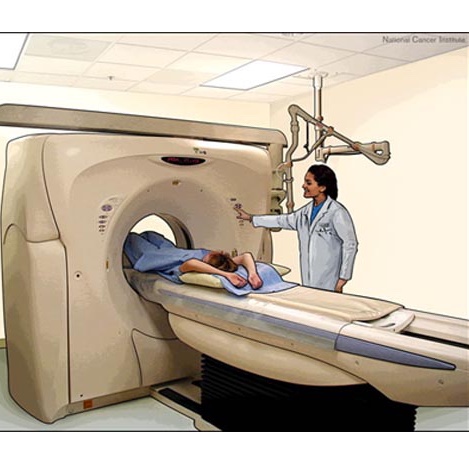
Image courtesy of the NCI
Radiotracers
18F-FDG
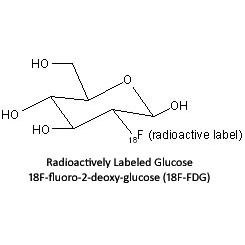
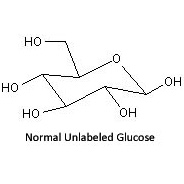
The most common tracer used for PET scans is 18F-fluoro-2-deoxy-glucose (18F-FDG), which is a radioactively labeled form of glucose. Glucose is a simple sugar that is the body's main source of energy and it is carried throughout the body in the bloodstream. Because all cells need energy to properly function and divide, glucose is found in every tissue and organ. When a cell needs energy, it collects glucose and processes it (via glycolysis and respiration) into a usable form of energy. PET scans take advantage of this process to create images. Cancer cells tend to use much more glucose than normal cells. Therefore, cancer cells (and tumors) collect more of the radiotracer and appear as a different color on the resulting images. The radiotracer 18F-FDG is frequently used because it is readily transported into cells. Once in cells, the chemical is phosphorylated into FDG-6-phosphate. The newly created molecule (FDG-6) is trapped within the cell and will no longer participate in metabolism.1
18F-FDG is an unstable molecule because it contains excess protons and once inside the body it begins to break down. As it breaks down it emits positrons, a positive electron, which break down further, releasing 2 equivalent photons in opposite directions. These photons are detected by a camera inside the PET unit, producing a high-resolution 3 dimensional image.1, 2
Disadvantages to 18F-FDG Use
18F-FDG is readily absorbed by macrophages, neutrophils, and active muscle cells. This may result in false positive test results, particularly in areas of inflammation and infection. Younger patients often give false negatives because of increased uptake in areas such as the brain, urinary system, thymus, and in smooth or striated muscle. False negatives can also occur when tumors are slow growing and absorb less glucose.2Watch a video explaining false positives and negatives in medical testing.
Other Radiotracers
The energy pathway identified by FDG is used by all cells, making this radiotracer useful in many cancer types. There are many different radiotracers used in PET scans that take advantage of other cellular processes. These are used to detect specific cancer types and to study other disease processes, like heart disease and Alzheimer's disease. Information on other radiotracers and their use can be found in the Molecular Imaging and Contrast Agent Database. New tracers are under development and promise to be more specific and produce more effective images with increased specificity, sensitivity, and overall accuracy.3
Pet scans take advantage of the fact that cancer cells use lots of sugar to grow. An altered form of sugar (shown in the animation above as a candy bar) is injected. PET scans detect when it collects in tumors
The Exam
Scheduling
When you are scheduling your exam be sure to mention if you:
- are diabetic
- have asthma
- are breast feeding
- are pregnant or think you are pregnant
- have a fear of enclosed spaces (claustrophobia)
- have previously had an allergic reaction to the tracer used in the exam
- NOTE:You should not schedule any other tests that use radioactive material for the same day
Day of exam
There are special instructions to follow the day of your PET exam:
- Drink plenty of water, but do not eat or drink anything (except water) for 6 hours before your exam
- Take your medications normally and drink them with ample water
- Make sure you arrive at the imaging center on time, the chemicals in the tracer break down rapidly and if you are late, the images may not be as good
- Wear loose fitting clothing
- Do not wear any jewelry; watches, chains, rings, piercings, etc.
- Prepare to be at the center for around 2 ½ hours
- NOTE: If you are a diabetic there are special rules you need to follow before the exam. You should follow your normal daily routine, eat small meals and take your insulin as usual. Your blood sugar should be between 100 and 200 mg/dL and your blood may be drawn to ensure this.
During
A nurse will start an IV and the tracer compound will be injected into a vein. You will be moved to a quiet, dark room where you will lie still for a specified amount of time, usually about 1 hour. During this period your body will completely absorb and distribute the tracer compound. In many cases you will be asked not to speak to prevent the compound from collecting in your tongue and vocal chords. You will then lie down on a padded table that will slide into the large opening in the PET machine. A technologist will position you (most likely with your arms placed above your head) to obtain the most accurate image and you will be asked to lie completely still during the entire scan, any movement may distort the image. The scan may last anywhere from 30 minutes to 1 ½ hours, if you have trouble staying still for long periods of time you may be sedated.
After
You should not be bothered by any side effects after the exam. You will be encouraged to drink plenty of fluids to help flush any remaining tracer from your body. If you were sedated you will need to arrange for someone to drive you home.
PET Imaging by Cancer Type
Below is a table describing the usefulness of 18F-FDG (18F-fluorodeoxyglucose) PET scanning with repect to diagnosis, staging, prognosis, treatment planning and response to therapy for several cancer types.
| Cancer Type | PET Scan Usage |
| Bladder | Not used for bladder cancer, because of 18F-FDG collects in the bladder and urinary tract making images very hard to interpret. |
| Brain | PET has limited use with brain cancer because normal brain tissue and cancerous tissue can have similar glucose uptake levels resulting in difficulty interpreting brain images. Other radiotracers are being investigated. |
| Breast |
PET has shown great potential in diagnosis of primary and recurrent disease, staging, prognosis and response to treatment. But, PET is not as accurate as mammography for primary screening, so it can't replace mammography at this point. A 2021 study showed that it may be possible to use PET to identify women whose breast cancer will respond to hormonal treatments.4 |
| Cervical | Limited role in the staging of cervical cancer, but may be useful in prognosis after treatment. |
| Colorectal | PET is useful in the diagnosis of recurrent colorectal cancer, with a sensitivity and specificity of 97% and 76%, respectively. There are other disorders of the bowel that cause increased uptake of FDG, causing image interpretation problems. |
| Endometrial | PET is able to detect recurrence during and after treatment with a sensitivity of 96-100% and a specificity of 78-88%. |
| Germ Cell Tumors | Use still in the early stages, but at this point it can effectively evaluate the presence of residual disease after therapy. |
| Head and Neck | PET is useful in diagnosis, assessment of response to treatment, prognosis and diagnosis of relapse. PET was found to be more sensitive than CT (94-100% for PET vs 77-91% for CT). |
| Lymphoma | PET is useful in detection of disease, with a higher sensitivity (94-100%) than CT (77-91%). PET is also useful in diagnosis, assessment of response to treatment, prognosis, and diagnosis. |
| Lung | PET scan is useful in diagnosis, staging, prognosis and radiotherapy. PET was found to be comparable to fine needle aspiration (FNA) for diagnosis |
| Melanoma | Not shown to be useful in primary staging. Can play a large role in diagnosis of relapse with a sensitivity, specificity, and accuracy all greater than 70%. |
| Non-Hodgkin's Lymphoma (NHL) | PET is capable of staging intermediate and high-grade NHL and also may be able to help in predicting treatment response. |
| Oesophageal | PET was found to be more accurate than CT and ultrasound, PET 82% accuracy compared to CT and ultrasound 64% accuracy, in detection of metastatic disease. Also found to be more accurate in nodal staging and may be useful in prognosis. |
| Ovarian | PET is useful in providing information about staging, especially when combined with CT. |
| Prostate | Imaging with PET alone has not been useful in prostate cancer imaging, but other options are currently under research. |
| Renal (Kidney) | PET shows nothing promising in management of renal cancer, but has some limited ability to stage metastatic disease. |
| Thyroid | PET was found more accurate than MRI and CT in detecting metastasis, with a sensitivity of 82-95% and a specificity of 83-95% |
All the information in this table was obtained from a review published in Clinical Oncology in 2007.2
Learn more about sensitivity and specificity of medical tests
Learn more about cancer staging
- 1ab ME Phelps. Molecular imaging with positron emission tomography. Annual Review of Nuclear and Particle Science. 2002; 52: 303-338.
- 2abc KA Wood, PJ Hoskin, MI Saunders. Positron Emission Tomography in Oncology: A Review. Clinical Oncology. 2007 19: 237-255. [PUBMED]
- 3 JF Vansteenkiste. Imaging in lung cancer: positron emission tomography scan. European Respiratory Journal. 2002; 19: Suppl. 35, 49s-60s. [PUBMED]
- 4 Dehdashti, F., Wu, N., Ma, C.X. et al. Association of PET-based estradiol-challenge test for breast cancer progesterone receptors with response to endocrine therapy. Nat Commun 12, 733 (2021). https://doi.org/10.1038/s41467-020-20814-9
