In general, tumors can be cancerous (malignant) or non-cancerous (benign). Thyroid cancer refers to malignant tumors, originating in the thyroid gland, which can spread (metastasize) to other places in the body.

The most common types of thyroid cancers are differentiated thyroid cancers (DTC). Compared with poorly differentiated and undifferentiated thyroid cancer cells, differentiated thyroid cancer cells look more like normal thyroid cells under a microscope and are more likely to have a better prognosis (less dangerous). There are several types of differentiated thyroid cancer.1, 2
- Papillary thyroid carcinoma (PTC) – This type of thyroid cancer is responsible for approximately 80% of all thyroid cancer cases and tends to grow very slowly and is rarely fatal. It usually develops in only 1 of the 2 lobes of the thyroid gland and often spreads to lymph nodes in the neck.
- Follicular thyroid carcinoma (FTC) – This type of thyroid cancer is responsible for approximately 10% of all thyroid cancer cases. FTC tends to spread to the lungs and bones through the bloodstream rather than spreading to the lymph nodes.
- Hurthle cell carcinoma– This type of thyroid cancer is responsible for approximately 3% of all thyroid cancer cases and is typically harder to locate with radioactive iodine, resulting in a relatively worse prognosis than the other two types of differentiated thyroid cancer.
The following types of thyroid cancers (poorly differentiated and undifferentiated) originate from follicular cells and are less common than differentiated thyroid cancers.1, 2
- Medullary thyroid carcinoma(MTC) – This type of poorly differentiated thyroid cancer is responsible for about 4% of all thyroid cancer cases and develops from the thyroid gland's parafollicular cells (C cells), which produce calcitonin to help control blood calcium levels. There are 2 types of MTC:
- Sporadic MTC– This type of MTC is responsible for about 80% of all MTC cases, does not run in families, and typically occurs in older adults.
- Familial MTC– This type of MTC is responsible for about 20% of all MTC cases, is inherited (runs in families), and often develops during childhood. Familial MTC is linked with an increased risk for developing other types of tumors.
- Anaplastic thyroid carcinoma (ATC) – This type of undifferentiated thyroid cancer is responsible for about 2% of all thyroid cancer cases. These cancer cells do not look like normal thyroid cells. Anaplastic carcinoma tends to spread quickly into the neck and other parts of the body, making it very difficult to treat.
The American Cancer Society estimates that there will be about 43,720 new thyroid cancer cases in 2023, with 31,180 in women and 12,540 in men. About 2,120 people are expected to die from thyroid cancer in 2023.3
Please visit the following sections to learn more about thyroid cancer:
- Anatomy and function of the thyroid
- Thyroid cancer risk factors
- Thyroid cancer prevention
- Thyroid cancer symptoms
- Thyroid cancer detection and diagnosis
- Thyroid cancer staging
- Thyroid cancer tumor biology
- Thyroid cancer treatment
- Thyroid cancer resources
- Thyroid cancer section summary
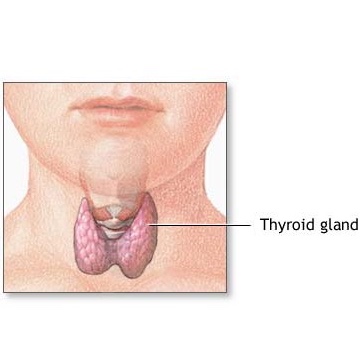
Anatomy and Function of the Thyroid
The thyroid gland is a butterfly-shaped hormone gland located below the larynx (voice box). It consists of 2 lobes (left and right) that wrap around the windpipe. As a part of the body's endocrine system, the thyroid gland produces hormones that regulate growth and metabolism in the body.4 Hormones are chemical messengers produced by endocrine glands that travel through the bloodstream to tissues and organs. They affect nearly every cell in the body and regulate numerous bodily processes, such as growth, metabolism, reproduction, mood, and more. 5, 6 Calcitonin, an example of a thyroid hormone, is produced by the thyroid gland's parafollicular cells (C cells) and regulates blood calcium levels. 7
Risk Factors
While certain types of thyroid cancer have been linked to various inherited conditions, as described below, the direct cause of most thyroid cancers is currently unknown. The following is a list of some of the known risk factors for developing thyroid cancer. These risk factors are expanded upon, below. Note that having a risk factor does not necessarily mean an individual will develop thyroid cancer.1
- Gender and age
- Low iodine intake
- Radiation
- Genetic predisposition
Gender and age
Although the reasons are currently unclear, women are three times more likely to develop thyroid cancer than men. Thyroid cancer can occur at any age, but women tend to develop thyroid cancer at an earlier age. Most women are diagnosed with thyroid cancer in their 40s or 50s, while most men are diagnosed in their 60s or 70s.1
Low iodine intake
Iodine is an element that is required by the body to synthesize important thyroid hormones. Most people in the United States consume sufficient amounts of iodine from iodized salts and other foods. Studies indicate that inadequate iodine intake will result in conditions that promote thyroid tumor growth. Such conditions include increased stimulation from thyroid-stimulating hormone (TSH), increased thyroid cell proliferation, increased angiogenesis (blood vessel formation), and more.8
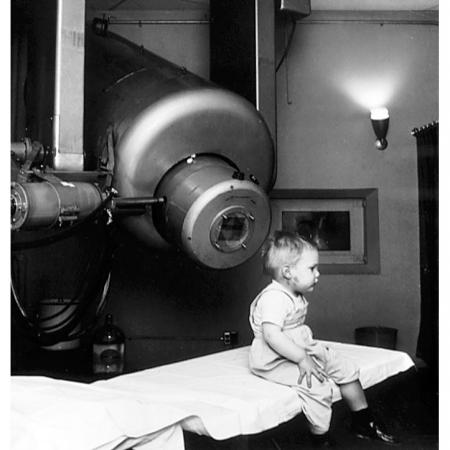
Radiation
The thyroid gland is one of the most radiosensitive organs in the body and is especially sensitive in children. Studies conducted on survivors of atomic bomb explosions and people who have received radiation therapy suggest that radiation is a risk factor for thyroid cancer. Moreover, early-life exposure to radiation, especially head and neck radiation, increases the risk in an individual for developing thyroid cancer. Sources of medical radiation exposures include X-rays, radiation therapy, CT scans, and more.9
For more information on radiation therapy, visit CancerQuest's page on radiation therapy.
Genetic Predisposition
Most cases of thyroid cancer are not thought to be due to an inherited susceptibility. However, certain types of thyroid cancers are linked to inherited medical conditions.1
- Approximately 1 out of 3 medullary thyroid cancer (MTC) cases result from the inheritance of the mutated RET gene. These cases are known as familial medullary thyroid carcinoma (FMTC). Having a family history of FMTC significantly increases an individual’s risk of developing MTC. Inherited forms of MTC, like FMTC, often develop during childhood or early adulthood.
- Individuals who have familial adenomatous polyposis (FAP) are at an increased risk of developing colon cancer and papillary thyroid cancer.
- Individuals with Cowden disease are at an increased risk of developing cancers of the thyroid, uterus, breasts, and more. Cowden disease is linked to defective PTEN genes.
Prevention
Although the direct cause of most thyroid cancers is currently unknown, certain factors may increase an individual's risk for developing thyroid cancer. The following may help lower these risks.1
- Avoiding radiation exposure in childhood, unless absolutely necessary
- Removing the thyroid gland in children who have tested positive for the mutated gene associated with familial medullary thyroid cancer (FMTC).
For more information on radiation therapy, visit CancerQuest’s page on radiation therapy.
Symptoms
Thyroid cancers are best treated at their early stages, so it is important for an individual to see a doctor if he/she has these symptoms. However, while the symptoms listed below are associated with thyroid cancer, they could also be due to other conditions.1
- Lump found in the neck
- Swelling in the neck
- Pain in the front of the neck
- Persistent hoarseness or voice changes
- Swallowing difficulties
- Persistent cough not due to a cold
Detection and Diagnosis
If an individual suspects he/she may have thyroid cancer, he/she should consult an oncologist and/or an endocrinologist (a doctor who specializes in the treatment of endocrine disorders). The doctor will ask the patient about his/her health history and may choose to conduct further tests to find out more information. The following are some examples of tests that may be performed.1
Physical exams
During physical exams, doctors will feel (palpate) for growths and indications of thyroid tumors. They will pay attention to the size and firmness of the thyroid as well as the presence of any enlarged lymph nodes in the neck.
MRI scans
MRI scans use radio waves instead of x-rays to detect thyroid cancer. Because MRI scans can provide detailed images of soft tissues, such as the thyroid, these scans are usually the preferred imaging method.
For more information, visit CancerQuest's page on MRI scans.
Ultrasound
An ultrasound uses sound waves to determine if thyroid nodules are solid or liquid-filled. Liquid-filled thyroid nodules are less likely to be cancerous. These scans can also help determine the number and size of these nodules.
For more information, visit CancerQuest's page on ultrasounds.
CT scans
CT scans use x-rays to help determine a tumor’s shape, size, and position. These scans can also help determine if the cancer has spread to other locations.
For more information, visit CancerQuest's page on CT scans.
PET scans
Positron Emission Tomography (PET) scans to track the movement of tagged chemicals in the body. PET images are not as detailed as CT scan images and cannot provide precise information about a tumor's shape, size, and position. PET scans can be used to identify the general location of a tumor and the location(s) of where the cancer has spread (metastasized).
For more information, visit CancerQuest's page on PET scans.
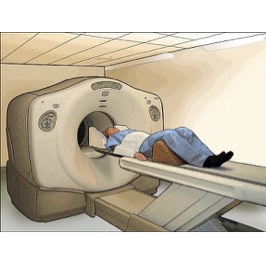
Image courtesy of the NCI
Lab tests
While blood tests alone cannot determine if a thyroid nodule is cancerous, these tests can provide valuable information regarding thyroid gland function and help determine which imaging tests to use. These blood tests may test for a patient’s thyroid-stimulating hormone (TSH) levels, T3 and T4 thyroid hormone levels, thyroglobulin levels, calcitonin levels, and carcinoembryonic antigen (CEA) levels.
For additional information on cancer detection and diagnosis tests, visit CancerQuest's page on cancer detection and diagnosis.
Staging
Staging allows doctors to figure out the degree to which the cancer has spread (metastasized) so that they will be able to work with the patient to develop a treatment plan. Staging is most often done during surgery, where a surgical oncologist takes tissue samples from targeted regions, for analysis. The most common staging system used for thyroid cancer is TNM staging. This system categorizes thyroid cancer based on the size and location of the cancer. For information on TNM staging, visit CancerQuest's page on TNM staging.
The following is a general summary of the stages of thyroid cancer.
- Stage I: The cancerous tumor is found only in the thyroid and is smaller than or equal to 2 centimeters.
- Stage II: The cancerous tumor is found only in the thyroid and is larger than 2 centimeters but no larger than 4 centimeters.
- Stage III: The cancerous tumor can be either of the following:
- Larger than 4 centimeters and found only in the thyroid
- Any size and spread to tissues just outside the thyroid or to the lymph nodes near the trachea or larynx (voice box)
- Stage IV: This is the most advanced stage of thyroid cancer. Cancer cells have spread (metastasized) beyond the thyroid, to nearby/distant lymph nodes and organs.
Tumor Biology
Studies have identified several genes and pathways that are linked to the development and spread of thyroid cancer. Identification of these genes has been crucial in the development of drugs to treat the disease. Genetic alterations of BRAF and RAS and RET/PTC rearrangements are found in over 70% of patients with papillary thyroid carcinoma (PTC), the most common type of thyroid cancer. Genetic alterations of RAS and PAX/PPARϒ are found in approximately 50% of patients with follicular thyroid carcinoma (FTC), the second most common type of thyroid cancer. The following is a list that includes some of the genes and pathways involved in thyroid cancer development.2
MAPK pathway
The mitogen-activated protein kinase (MAPK) pathway is an important cell-signaling pathway that regulates cell growth, division, differentiation, and survival. Genetic and epigenetic alterations of the Ras-Raf-MEK-MAPK-ERK have been implicated in thyroid cancer development.10, 11
BRAF gene
This gene encodes for a serine-threonine kinase that is a member of the Raf family of proteins. Studies have found that an activating mutation in BRAF results in the constitutive activation of Braf kinases such that Braf kinases are always actively inducing the MAPK signaling pathway. Studies suggest a direct link between these BRAF mutations and aggressive papillary thyroid cancer growth.12
RAS gene
This gene encodes for the Ras G-protein. The Ras G-protein is responsible for controlling gene transcription, which then regulates cell growth and differentiation. Mutations in Ras frequently result in Ras proteins that are always active, leading to genomic instability, induction of other genetic mutations, and transformation of cells into cancerous cells. Ras mutations have been observed in papillary thyroid carcinoma, follicular thyroid carcinoma, and undifferentiated thyroid cancers. Ras mutations have also been found in benign thyroid tumors.2
RET/PTC rearrangements
The RET gene encodes for a membrane-bound tyrosine kinase receptor. This gene is expressed in high levels in calcitonin-producing parafollicular cells (C cells) of the thyroid gland. Studies have found that certain rearrangements of the RET gene lead to fusion genes that result in the RET kinases that are always active. These rearrangements are known as RET/PTC rearrangements due to their association with papillary thyroid cancer development.2, 13
PAX8/PPARϒ rearrangements
The PAX8 gene encodes for a transcription factor that is important for thyroid development during embryogenesis. The PPARϒ gene encodes for nuclear receptor proteins, which are transcription factors that regulate gene expression. PAX8/PPARϒ rearrangements occur due to a translocation between chromosomes 2 and 3. In other words, these rearrangements occur when breaks in chromosome 2 and chromosome 3 result in the formation of two “new” chromosomes that have new combinations of genes. 2, 14This translocation results in an increased expression of the PAX8/PPARϒ fusion protein, which acts as an oncoprotein, transforming cells into cancer cells. 15PAX8/PPARϒ rearrangements have been observed in follicular thyroid carcinomas and follicular adenomas.16, 17, 18
TP53 gene
This gene encodes for the tumor suppressor protein, p53, which is in charge of regulating cell division and cell death (apoptosis). While p53 mutations are rarely seen in thyroid cancers, loss of p53 function is very common. Studies have found that loss of p53 activity enhances thyroid cancer development and results in the loss of differentiation in thyroid tumors.2, 19
Treatment
Treatment options for thyroid cancer depend on the tumor's location, the degree to which the tumor is affecting thyroid functions, and the patient's health history. Some treatment options include chemotherapy, radioiodine therapy, radiation therapy, surgery, and targeted therapies.
Since CancerQuest's focus is on the cancer's biology and the biology of possible treatments, we do not give detailed treatment guidelines. Instead, we link to organizations in the U.S. that do generate treatment guidelines:
- Learn about the treatments recommended by the National Comprehensive Cancer Network (NCCN) for Thyroid Cancers.
- Learn about how cancer treatments work at CancerQuest's page on cancer treatments.
For information about clinical trials:
- Information about clinical trials from CancerQuest
- Information about clinical trials from the National Cancer Institute
- Information about clinical trials from Georgia Clinical Trials Online
Thyroid Cancer Resources
Risks for Thyroid Cancer
Thyroid Cancer Risk Factors (ACS)
Moffitt Cancer Center: Thyroid Cancer Risk Factors
Detection and Diagnosis of Thyroid Cancer
Winship Cancer Institute: Thyroid Cancer
Thyroid Cancer: What You Need To Know
Detailed Guide to Thyroid Cancer (ACS)
Thyroid Cancer Treatments
Thyroid Cancer Treatment (NCI)
How is Thyroid Cancer Treated? (ACS)
Thyroid Cancer Treatments (Mayo Clinic)
Thyroid Cancer Survivorship
Thyroid Cancer Survivors' Association
Long Term Risks for Thyroid Cancer Survivors
Radioactive Iodine Risks and Side Effects (ACS)
Possible Side Effects of Thyroid Hormone Therapy (ACS)
Possible Side Effects of External Beam Radiation for Thyroid Cancer (ACS)
Effects of Thyroid Cancer Chemotherapy (ACS)
International Thyroid Cancer Resources
Thyroid Cancer (Cancer Research UK)
Thyroid Cancer (Macmillan Cancer Support UK)
Cancer Council Australia: Thyroid Cancer
Thyroid Cancer (Cancer Australia)
Thyroid Cancer (The Australia Thyroid Foundation)
Section Summary
Introduction
- The death rate from thyroid cancer has remained relatively stable and low throughout the years, when compared with most other cancers.
- Approximately 67% of thyroid cancer diagnoses occur in people younger than 55 years of age, and approximately 2% of thyroid cancer diagnoses occur in children and teens.
Types of Thyroid Cancer
- The most common types of thyroid cancers are differentiated thyroid cancers. There are several types of differentiated thyroid cancer: papillary carcinoma, follicular carcinoma, and Hurthle cell carcinoma.
- The following types of thyroid cancers are less common than differentiated thyroid cancers: medullary thyroid carcinoma (MTC) and anaplastic carcinoma.
Risk Factors
- Studies indicate that inadequate iodine intake will result in conditions that promote thyroid tumor growth.
- Early-life exposure to radiation, especially head and neck radiation, increases the risk in an individual for developing thyroid cancer.
- Approximately 1 out of 3 medullary thyroid cancer (MTC) result from the inheritance of the mutated RET gene.
Detection
- Several medical tests can be used to detect or rule out a thyroid tumor. Examples include: physical exams, MRI scans, ultrasound scans, PET scans, and CT scans.
Staging and Pathology
- The T/N/M system is one of the most common methods used for thyroid cancer staging.
- The T/N/M system assigns a degree of severity based on the size and location of the cancer.
Treatment
- Treatments differ depending on specific factors, such as the patient’s age, patient’s health conditions, cancer stage, tumor location, and more.
- Treatments can include surgery, radioiodine therapy, radiation therapy, chemotherapy, and targeted therapies.
- 1abcdefgh Thyroid Cancer Detailed Guide. American Cancer Society. [http://www.cancer.org/cancer/thyroidcancer/detailedguide/index]
- 2abcdefg Omur O, Baran Y. An update on molecular biology of thyroid cancers. Crit Rev Oncol Hematol. 2014 Jun;90(3):233-52. doi: 10.1016/j.critrevonc.2013.12.007. Epub 2013 Dec 18. [PUBMED]
- 3 American Cancer Society.Cancer Facts & Figures 2023. Atlanta: American Cancer Society. (2023). 取读于 从 https://www.cancer.org/research/cancer-facts-statistics/all-cancer-facts-figures/2023-cancer-facts-figures.html
- 4 Mullur, R., Liu, Y.-Y., & Brent, G. (2014). Thyroid hormone regulation of metabolism. Physiological reviews, 94(2), 355–82. http://doi.org/10.1152/physrev.00030.2013 (Original work published 2014年4月) [PUBMED]
- 5 Zhang J, Lazar MA. The mechanism of action of thyroid hormones. Annu Rev Physiol. 2000;62:439-66. [PUBMED]
- 6 Hormones. Medline Plus. U.S. National Library of Medicine. [http://www.nlm.nih.gov/medlineplus/hormones.html]
- 7 Hirsch PF, Lester GE, Talmage RV. Calcitonin, an enigmatic hormone: does it have a function? J Musculoskelet Neuronal Interact. 2001 Jun;1(4):299-305. [PUBMED]
- 8 Knobel M, Medeiros-Neto G. Relevance of iodine intake as a reputed predisposing factor for thyroid cancer. Arq Bras Endocrinol Metabol. 2007 Jul;51(5):701-12. [PUBMED]
- 9 Schonfeld SJ, Lee C, Berrington de González A. Medical exposure to radiation and thyroid cancer. Clin Oncol (R Coll Radiol). 2011 May;23(4):244-50. doi: 10.1016/j.clon.2011.01.159. Epub 2011 Feb 5. [PUBMED]
- 10 Xing M. Recent advances in molecular biology of thyroid cancer and their clinical implications. Otolaryngol Clin North Am. 2008 Dec;41(6):1135-46, ix. doi: 10.1016/j.otc.2008.07.001. [PUBMED]
- 11 Kondo T, Ezzat S, Asa SL. Pathogenetic mechanisms in thyroid follicular-cell neoplasia. Nat Rev Cancer. 2006 Apr;6(4):292-306. [PUBMED]
- 12 Nikiforov YE, Nikiforova MN. Molecular genetics and diagnosis of thyroid cancer. Nat Rev Endocrinol. 2011 Aug 30;7(10):569-80. doi: 10.1038/nrendo.2011.142. [PUBMED]
- 13 Nikiforov YE. RET/PTC rearrangement in thyroid tumors. Endocr Pathol. 2002 Spring;13(1):3-16. [PUBMED]
- 14 Laury AR, Perets R, Piao H, Krane JF, Barletta JA, French C, Chirieac LR, Lis R, Loda M, Hornick JL, Drapkin R, Hirsch MS. A comprehensive analysis of PAX8 expression in human epithelial tumors. Am J Surg Pathol. 2011 Jun;35(6):816-26. doi: 10.1097/PAS.0b013e318216c112. [PUBMED]
- 15 Gregory Powell J, Wang X, Allard BL, Sahin M, Wang XL, Hay ID, Hiddinga HJ, Deshpande SS, Kroll TG, Grebe SK, Eberhardt NL, McIver B. The PAX8/PPARgamma fusion oncoprotein transforms immortalized human thyrocytes through a mechanism probably involving wild-type PPARgamma inhibition. Oncogene. 2004 Apr 29;23(20):3634-41. [PUBMED]
- 16 French CA, Alexander EK, Cibas ES, Nose V, Laguette J, Faquin W, Garber J, Moore F Jr, Fletcher JA, Larsen PR, Kroll TG. Genetic and biological subgroups of low-stage follicular thyroid cancer. Am J Pathol. 2003 Apr;162(4):1053-60. [PUBMED]
- 17 Nikiforova MN, Lynch RA, Biddinger PW, Alexander EK, Dorn GW 2nd, Tallini G, Kroll TG, Nikiforov YE. RAS point mutations and PAX8-PPAR gamma rearrangement in thyroid tumors: evidence for distinct molecular pathways in thyroid follicular carcinoma. J Clin Endocrinol Metab. 2003 May;88(5):2318-26. [PUBMED]
- 18 Marques AR, Espadinha C, Catarino AL, Moniz S, Pereira T, Sobrinho LG, Leite V. Expression of PAX8-PPAR gamma 1 rearrangements in both follicular thyroid carcinomas and adenomas. J Clin Endocrinol Metab. 2002 Aug;87(8):3947-52. [PUBMED]
- 19 Malaguarnera R, Vella V, Vigneri R, Frasca F. p53 family proteins in thyroid cancer. Endocr Relat Cancer. 2007 Mar;14(1):43-60. [PUBMED]