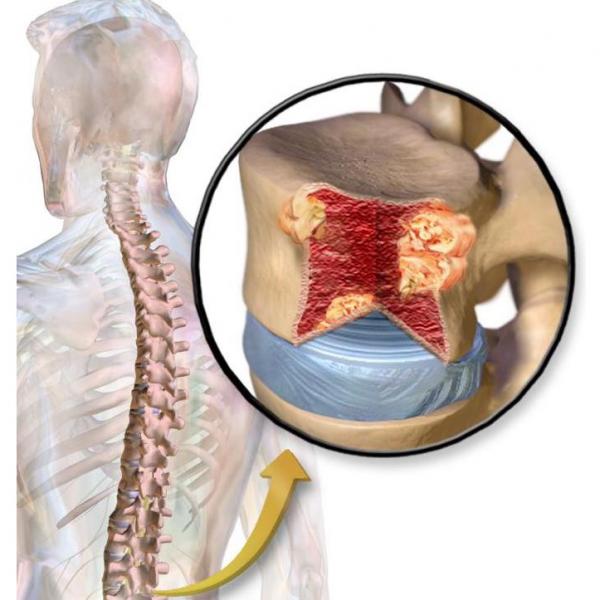
Myeloma growing in a bone in the spine.1
Myeloma is a cancer that affects B cells, the immune cells responsible for the production of antibodies. Normal B cells develop in bone marrow This is also where myeloma grows. Multiple myeloma arises when the cancer cells travel through the body and form tumors in several different bones. Affected bones may become brittle as the cancer cells reproduce and alter the marrow.2
Watch the full interview with multiple myeloma patient Ginny Johnston.
In 2023, the American Cancer Society estimates that 35,730 new myeloma cases will be diagnosed and 12,590 cancer deaths due to myeloma will occur.3
Below is a list of the information found within this section:
- Immune Cells
- Risk Factors
- Symptoms
- Detection and Diagnosis
- Pathology Report and Staging
- Tumor Biology
- Treatment
- Multiple Myeloma Resources
- Section Summary
Immune Cells And Multiple Myeloma
The immune system recognizes and eliminates foreign objects (like splinters) and disease-causing agents (including bacteria and viruses). Multiple myeloma is a cancer of B lymphocytes, a type of immune cell. In adults, B cells form and mature in the bone marrow. When activated, B cells produce Y-shaped proteins (antibodies) that are part of the immune response. Antibodies bind to their targets helping clear them from the body. The many different B cells in our bodies each make only one type of antibody. B cells that have become activated to produce antibodies are called 'plasma cells'.4
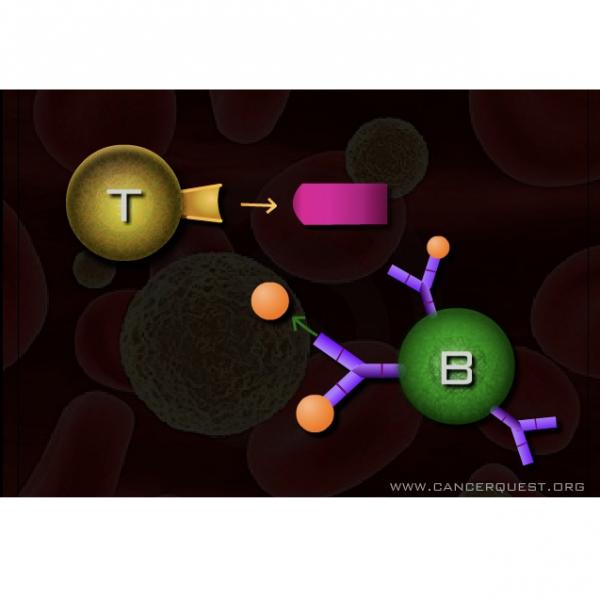
In multiple myeloma a plasma B cell becomes genetically damaged and reproduces (proliferates) uncontrollably. The cancerous cells over-produce antibodies that may accumulate in the bone marrow. The myeloma cells also stimulate bone cells called osteoclasts. Osteoclasts produce proteins that dissolve the bone and cause some of the symptoms associated with the disease, including pain and disfigurement. Because B cells normally move around the body, the cancerous cells are able to get in the bloodstream and spread to other locations (metastasis) is very common. Frequently, multiple tumors are found in bones.2
Risk Factors
Multiple myeloma (MM) is more common in men than women. The ratio of male to female diagnosis is about 1.4:1. The American Cancer Society predicts that 17,530 men and 14,740 women will be diagnosed with this disease in 2020. Multiple myeloma is also twice as common in African Americans than in Caucasians. 5The cause for this difference is unknown.
Recognized risk factors include5, 6:
- Age - The risk of developing MM is higher for the elderly. The median age at diagnosis is 69.
- Gender - Men are more likely to develop MM than women.
- Race - African Americans are more likely to develop MM than other ethnicities.
- Radiation exposure
- Family history - Prior family history of myeloma increases risk of MM development.
- Jobs with exposure to petroleum products
- Obesity - Studies suggest that obesity may increase risk.
- Other plasma cell diseases - People with diseases affecting B cells, including plasmacytoma and monoclonal gammopathy of unknown significance (MGUS) are more likely to develop MM.
Symptoms
Multiple Myeloma is often difficult to diagnose because the vague symptoms that may be present in the early stages of the disease are often mistaken for other illnesses. In many patients, symptoms do not appear until the disease is at an advanced stage. Routine blood tests may be able to detect abnormal blood protein levels.
Symptoms include:7
- bone pain
- chronic fatigue
- blood cell (hematologic) abnormalities- i.e. anemia, a condition when the patient doesn't have enough healthy red blood cells
- nervous system abnormalities (neuropathy)
- repeated infections
- loss of kidney function (renal failure)
- elevated levels of calcium in the blood (hypercalcemia)
- unexplained weight loss
- elevated levels of antibodies (immunoglobulin) or other proteins in the blood and/or urine
Watch an interview about multiple myeloma survivor Ginny Johnston
Detection And Diagnosis
Multiple myeloma results in the overproduction of antibodies by B cells in the tumors. The antibodies can be detected in samples of blood or urine from the patient. Another protein present on the surface of B cells (β-2 microglobulin) is frequently elevated in multiple myeloma. Multiple myeloma may also be detected by bone marrow biopsies.8
The National Comprehensive Cancer Network (NCCN) recommends PET and CT scans. CT scan may detect alterations and damage to bone structures. A whole-body MRI is another option. MRI images provide valuable information and may allow for greater accuracy in diagnosis.8
Multiple myeloma is commonly found in the vertebrae, skull, pelvic bones, ribs, humerus, and femur. Dentists may help identify the disease if it affects the jaw region of the skull.
Gene expression profiling is under investigation as a way of categorizing multiple myeloma cases. Expression profiling is a way to categorize the cancer cells based on their biological properties. Profiling and molecular markers are increasingly important and common tools to guide treatment decisions.9, 10
Learn more about cancer detection methods. Methods covered include PET, CT, and MRI.
Pathology Report And Staging
The staging system used for multiple myeloma is the "International Staging System" or ISS. This system is less complex than the previous Durie-Salmon Staging System. Hemoglobin value, serum calcium value, bone disfiguration, low M-component production rates IgG value and IgA value, as well as uring light chain level are no longer included. Staging now is based only on levels of two blood proteins, serum albumin and β-2 microglobulin.11
- Stage 1: Serum β-2 Microglobulin less than 3.5mg/L and Serum Albumin greater than 3.5g/dL
- Stage 2: *not classified as either stage 1 or 3*
- Stage 3: Serum β-2 Microglobulin greater than 5.5mg/L
Tumor Biology
The malignant B plasma cells in Multiple Myeloma generally migrate to the bone marrow. Once in, they attach to the supporting structures and cells (matrix). The matrix supports the cells as they proliferate. Within the bone marrow, numerous growth factors and other proteins influence the growth of the cells.12
Some of the growth factors and cytokines that play a role in multiple myeloma are:
- Interleukin 6 (IL-6) - a cytokine secreted by T cells. Stimulates other white blood cells (leukocytes), including B cells.13
- Tumor Necrosis Factor alpha (TNFα) - a cytokine mainly secreted by macrophages. Stimulates the immune system and induces inflammation.
- Vascular Endothelial Growth Factor (VEGF) - a growth factor secreted by cells in the bone marrow. Promotes angiogenesis and therefore the growth of tumors.
- Insulin-like Growth Factor I (IGF-1) - a growth factor that activates the AKT pathway. Promotes growth and inhibits cell death.
- Stromal Derived Factor 1 alpha (SDF-1α) - a cytokine that regulates the migration of blood cells to the bone marrow.
- Hepatocyte Growth Factor (HGF) - a glycoprotein produced by cells in the bone marrow. Promotes the adhesion of cells to the matrix and may regulate cell migration.14
Genes that have been implicated in multiple myeloma include:
- PTTG-1 - a proto-oncogene coding for a transcription factor associated with progression in multiple myeloma2
- PI3K - a gene that codes for a kinase that promotes cell division.15
- AKT - a proto-oncogene. The protein product inhibits cell death.15
- GILZ - a tumor suppressor gene that promotes cell death when activated by glucocorticoids. It is inhibited by the activities of PI3K and AKT.15
Treatment
As our focus is on the biology of the cancers and their treatments, we do not give detailed treatment guidelines. Instead, we link to organizations in the U.S. that generate the treatment guidelines.
The National Comprehensive Cancer Network (NCCN) lists the following treatments for multiple myeloma:
- Drug Therapy16
- Proteasome inhibitors: bortezomib (Velcade®), etc.
- Immunomodulating agents: thalidomide, lenalidomide, pomalidomide
- Chemotherapy: melphalan, doxorubicin hydrochloride liposome (Doxil®), etc.
- Combination chemotherapy: often includes dexamethasone
- Monoclonal antibodies: daratumumab
- Bisphosphonates for bone disease
- Autologous Stem Cell Transplantation
Learn more about cancer treatments
Information about clinical trials:
- General clinical trial information from CancerQuest
- Click here for information about clinical trials from the National Cancer Institute.
- Click here for information about clinical trials from Georgia Clinical Trials Online.
Multiple Myeloma Resources
Risks for Multiple Myeloma
Risks: Multiple Myeloma (Mayo Clinic)
Risk Factors for Multiple Myeloma (ACS)
Detection and Diagnosis of Multiple Myeloma
Winship Cancer Institute: Multiple Myeloma Cancer Diagnosis and Staging Make an Appointment
Multiple Myeloma Treatments
Plasma Cell Neoplasms (Including Multiple Myeloma) Treatment (NCI)
Diagnosis and Treatment of Multiple Myeloma (Mayo Clinic)
Multiple Myeloma Survivorship
Multiple Myeloma Research Foundation
Long Term Risks for Multiple Myeloma Survivors
Multiple Myeloma: Side Effects
Multiple Myeloma Revlimid Side Effects
International Multiple Myeloma Resources
Multiple Myeloma International Foundation
European School of Haematology
Section Summary
Introduction
- Results from malignant B cells that migrate to the bone marrow.
- ACS estimates that 32,270 new cases of MM will be diagnosed and 12,830 deaths will be reported in a year.
- Only accounts for 1% of all cancers.
- Current 5-year relative survival rate is 53.9%.17
Anatomy
- B plasma cells are a type of differentiated lymphoid cell.
- Plasma cells normally produce antibodies, proteins that help combat various pathogens, and each cell produces a specific antibody.
- In MM, the cancerous plasma cells become uncontrollable and produce large amounts of non-helpful antibodies.
- The cells migrate to the bone marrow where they receive growth signals.
- Typically the tumor in the bone marrow spreads to other parts of the body.
Risk Factors
- The male to Female ratio of diagnoses is 1.4:1.
- ACS estimates 17,530 men and 14,740 women will be diagnosed in 2020.
- For reasons unknown, MM is twice as likely in African Americans as in Caucasians.
- Age, gender, race, radiation exposure, family history, working in petroleum-related industries, obesity, and other plasma cell diseases may also increase risk.
Symptoms
- Symptoms may not be apparent until a late stage of the disease.
- It is important to get routine blood work done.
- Symptoms may include: chronic pain in the bone, chronic fatigue, anemia, neuropathy, recurring infections, hypercalcemia.
Detection and Diagnosis
- Blood or urine tests can detect abnormalities in antibody-protein levels.
- NCCN recommends PET, CT, or MRI scans.
- Bone marrow biopsy is an option.
- Dental professionals can identify some cases (tumors in the jaw).
Staging and Pathology
- New staging system called the "International Staging System" is now used.
- The ISS is simpler than previous systems.
- Staging is now based on the levels of beta-2 microglobulin and albumin in the blood of the patient.
Multiple Myeloma Tumor Biology
- MM development is dependent on gene mutation and growth factors.
- The bone marrow provides growth signals to the tumor and prevents cell death.
- Some of the cytokines involved are: IL-6, TNFa, VEGF, IGF-1, SDF-1a, HGF
- Some of the genes involved are: PTTG-1, PI3K, AKT, GILZ
Treatment
- Treatment success is very dependent on the stage of the cancer
- A primary option is hemopoietic stem cell transplant
- Drug therapy with bortezomib (or other proteasome inhibitors), lenalidomide (or other immunomodulators), and doxorubicin is frequently used.
- 1 Graphic donated into the public domain by Blausen Medical Communications, Inc
- 2abc Chiriva-Internati M, Ferraro R, Prabhakar M, Yu Y, Baggoni L, Moreno J, Gagliano N, Portinaro N, Jenkins MR, Frezza EE, Hardwicke F, D'Cunha N, Kast W, Cobos E. "The pituitary tumor transforming gene 1 (PTTG-1): an immunological target for multiple myeloma." J Transl Med. 2008 Apr 2;6:15. [PUBMED]
- 3 American Cancer Society. Cancer Facts & Figures 2020. Atlanta, Ga: American Cancer Society; 2020 [https://www.cancer.org/content/dam/CRC/PDF/Public/8738.00.pdf]
- 4 Roitt IM, Brostoff J, Male DK. "Immunology" Gower Medical Publishing Ltd. 1985. London. Pg 2.3
- 5ab Cancer Facts and Figures 2010. American Cancer Society. [http://www.cancerquest.org/sites/default/files/assets/pdf/facts%26figures2010.pdf]
- 6 Alexander DD, Mink PJ, Adam HO, Cole P, Mandel JS, Oken MM, and Trichopoulos D. Multiple myeloma: A review of the epidemiologic literature. International Journal of Cancer. 2001; 120:40-61. [PUBMED]
- 7 American Cancer Society. "Detailed Guide: Multiple Myeloma". Copyright 2010 American Cancer Society. Site accessed October 2010. [http://www.cancer.org/Cancer/MultipleMyeloma/DetailedGuide/multiple-myeloma-detection]
- 8ab Schmidt GP, Schoenberg SO, Reiser MF, Baur-Melnyk A. "Whole-body MR imaging of bone marrow." Eur J Radiol (2005 Jul);55(1):33-40. [PUBMED]
- 9 Henry T. and R. Fonseca. "Genomics and proteomics in multiple myeloma and Waldenström macroglobulinemia." Curr Opin Hematol. 2007 Jul;14(4):369-74 [PUBMED]
- 10 PL Bergsagel. "Individualizing therapy using molecular markers in multiple myeloma." (2007) Clin Lymphoma Myeloma. Apr;7 Suppl 4:S170-4. [PUBMED]
- 11 Katzel JA, Hari P, Vesole DH. "Multiple myeloma: charging toward a bright future." CA Cancer J Clin. 2007 Sep-Oct;57(5):301-18. [PUBMED]
- 12 Hideshima T, Podar K, Chauhan D and KC Anderson. "Cytokines and signal transduction." (2005) Best Pract Res Clin Haematol. 18(4):509-24. [PUBMED]
- 13 Huston A and GD Roodman."Role of the microenvironment in multiple myeloma bone disease." (2006) Future Oncol. Jun;2(3):371-8 [PUBMED]
- 14 Holt RU, Fagerli UM, Baykov V, Ro TB, Hov H, Waage A, Sundan A, Borset M. "Hepatocyte growth factor promotes migration of human myeloma cells". Haematologica. 2008 Apr;93(4):619-22. [PUBMED]
- 15abc Grugan KD, Ma C, Singhal S, Krett NL, Rosen ST. "Dual regulation of glucocorticoid-induced leucine zipper (GILZ) by the glucocorticoid receptor and the PI3-kinase/AKT pathways in multiple myeloma." J Steroid Biochem Mol Biol. 2008 Jun;110(3-5):244-54. Epub 2008 Apr 20. [PUBMED]
- 16 National Comprehensive Cancer Network (NCCN) Clinical Practice Guidelines in Oncology. Multiple myeloma. 2019.
- 17 SEER Cancer Stat Facts: Myeloma. National Cancer Institute. Bethesda, MD, https://seer.cancer.gov/statfacts/html/mulmy.html