The American Cancer Society estimates that in 2023, 64,050 people will be diagnosed with pancreatic cancer and there will be 50,550 deaths. In the U.S. pancreatic cancer is the 4th overall cause of cancer-related deaths for both men and women.1
Please visit the following sections to learn more about pancreatic cancer:
- Anatomy of the Pancreas
- Types of Pancreatic Cancers
- Risk Factors For Pancreatic Cancer
- Symptoms of Pancreatic Cancer
- Pathology Report & Staging
- Detection and Diagnosis
- Pancreatic Cancer Tumor Biology
- Pancreatic Cancer Treatment
- Pancreatic Cancer Resources
- Section Summary
Anatomy of The Pancreas
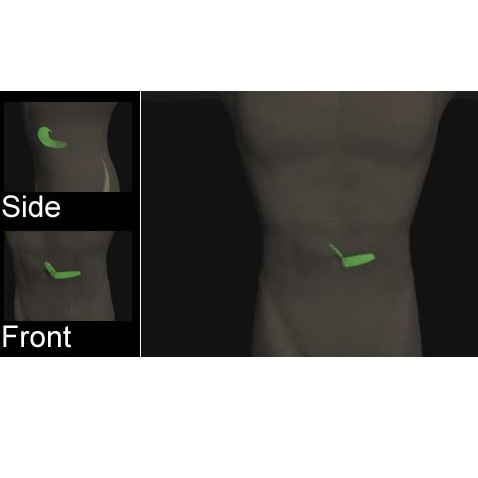
The pancreas is an oblong organ that lies behind the stomach in the abdomen. Its shape resembles a letter "J" that lies on its side with the hook pointing down. The pancreas plays an important role in digestion and has two main functions. It contains specialized (exocrine) cells that produce digestive enzymes which are secreted into the duodenum during digestion. Different endocrine cells secrete hormones such as insulin and glucagon to help regulate glucose metabolism.2
During digestion, cells in the epithelial lining of the small intestine release the hormones secretin and cholecystokinin (CCK) which act on the pancreas to stimulate its exocrine cells to produce digestive enzymes and bicarbonate ions. This collective digestive juice flows down the pancreatic ducts into the duodenum to aid the digestion of lipids and proteins.3
The exocrine epithelial cells are the cells of origin for most pancreatic tumors. Tumor formation and growth may hinder the ability of the pancreas to deliver its enzymes and digestive fluid into the small intestine and cause a broad spectrum of complications.
Types
The type of cancer is based on the cell type and location of the tumor in the pancreas. More than 95% of pancreatic cancers are adenocarcinomas of the exocrine pancreas.
- Adenocarcinoma - Cancer of the exocrine cells that line the pancreatic ducts. The majority of pancreatic cancers are of this type.
- Cystic Tumors - tumors that cause fluid-filled sacs in the pancreas. Most are benign.
- Acinar Cell Cancers - tumors that form on the ends of the pancreatic ducts in the cells that produce enzymes.
- Sarcomas - tumors that form in the connective tissue that bonds together the pancreatic cells. This is very rare.
- Ampullary Cancers - cancer that develops in the ampulla of Vater (where pancreatic ducts and bile ducts merge).4
Learn more about the types of cancer
Most of the adenocarcinomas occur in the head of the pancreas (the section closest to the small intestine). This can interfere with the drainage of bile from the bile ducts coming from the liver and produce a yellowish coloration of the skin and eyes (jaundice). See the symptoms section for more details.
Risk Factors
There are both genetic predisposition and behavioral risk factors for pancreatic cancer.
Genetic Predisposition
There is no identified familial form of pancreatic cancer but there is a genetic link in about 5% of patients. A mutation in the p16 tumor suppressor gene has been associated with increased risk. Alterations in BRCA-2, a breast cancer susceptibility gene have been identified in families with multiple cases of pancreatic cancer. The rates of pancreatic cancer are slightly higher in men than in women.5, 6
Risk Factors
Age: most diagnoses are made between the ages of 60-80
Increased Body Mass Index (BMI): BMI is used to determine whether or not an individual is at a healthy weight. Overweight and obese people have higher BMI values. There is a correlation between increased BMI and pancreatic cancer.
Smoking: Pancreatic cancer rates in smokers are over twice that of non-smokers.
Diabetes: Abnormal function of the pancreas is associated with pancreatic cancer. In diabetes, the pancreas fails to produce adequate amounts of the hormone insulin.
Chronic Inflammation: Pancreatitis is the chronic inflammation of the pancreas. Chronic inflammation is associated with elevated levels of DNA damage and other factors that favor the development of cancer. When combined with smoking and the use of smokeless tobacco, pancreatitis is strongly linked to an increased risk of pancreatic cancer.7, 8
Prevention of Pancreatic Cancer
Antioxidants: Diet is thought to play a role in at least some cases of pancreatic cancer. Results of the European Prospective Investigation of Cancer (EPIC) study indicate that a diet high in the antioxidants vitamins C E, and selenium may significantly reduce the risk of pancreatic cancer.9
Symptoms
In its early stages, pancreatic cancer does not typically have many obvious symptoms. Often symptoms that are present are subtle and may not be noticed. For this reason, most pancreatic cancers are diagnosed at a late stage. Symptoms of pancreatic cancer include10:
- Jaundice: A yellowing of the eyes and skin. This is caused by the obstruction of the bile ducts that join the pancreatic ducts.
- Weight Loss: Loss of body weight for no apparent reason
- Pain in the abdomen and back: A dull pain in the abdomen that extends into the back. It may be worse after meals.
- Steatorrhoea: This is the passing of fatty stools. Because the stools contain a large amount of fat, they noticeably float in water.
- Glucose Intolerance: Abnormally high blood glucose levels.
Detection And Diagnosis
Currently, there are no methods of early detection for pancreatic cancer.
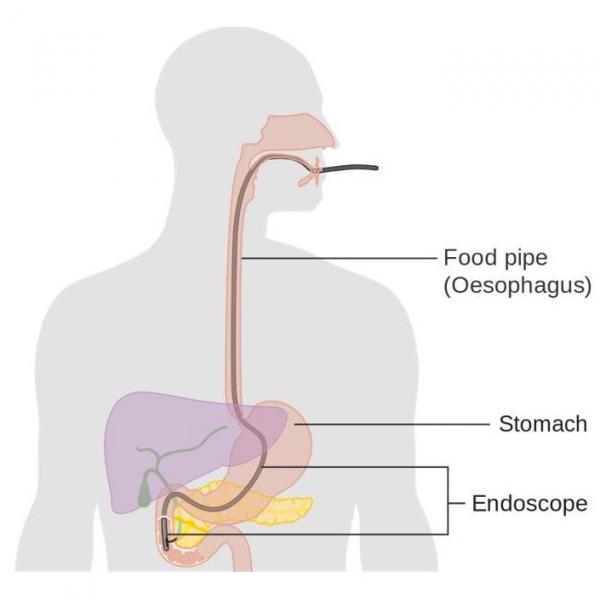
Pancreatic cancer is usually diagnosed via imaging techniques after the discovery of a mass or a dilated duct in the pancreas. Methods used to detect pancreatic cancer include CT scans and ultrasound. The imaging results help clinicians to determine the type and extend of the problem. Imaging results can also be used to assess treatment options. If there is no tangible mass in the pancreas, additional techniques such as endoscopic retrograde cholangiopancreatography (ERCP) may be used. This technique uses a combination of x-rays and an endoscope. The endoscope is used to inject a dye that enhances the x-ray image. Although a biopsy is not necessary prior to a surgical procedure, it is usually required prior to administration of adjuvant therapy.11, 12
Staging
Pancreatic cancer is assessed using the T,N,M staging system. This system measures the size of the primary tumor (T), the involvement of regional lymph nodes (N), and the presence of distant metastases (M) respectively. It is very important to determine the extent of the cancer growth to assess the possibility of surgical removal. Larger pancreatic cancers are less likely to be treated by surgery due to a reduced likelihood of success.
Learn more about the TNM staging system
Based on the staging results, pancreatic cancers can be classified into one of four categories:
- Resectable: These tumors may be removed surgically.
- Borderline Resectable
- Locally Advanced Unresectable
- Disseminated
This evaluation system is based on imaging results and allows the surgeon to judge the likelihood of success.11, 13
Tumor Biology
More than 90% of pancreatic cancers are not known to be associated with an inherited defect. The cancer develops via the accumulation of mutations that occur over time. The genes thought to be involved in the development of pancreatic cancer include:14
K-Ras
Ras is a proto-oncogene. The protein product of the gene is involved in cell signaling. When mutated in a way that makes the protein constantly active, Ras can cause uncontrolled cell growth. 75-90% of pancreatic cancers involve a point mutation in this gene.
PTEN
The PTEN protein is a tumor suppressor that removes phosphate groups from targets (it is a phosphatase). Mutations that cause loss of function reduce the ability of cells to control cell division pathways.
HER2/neu
This is a growth factor receptor that lies on the external surface (plasma membrane) of cells. This is often mutated and overactive in breast cancer and has also been found to be altered in pancreatic cancer.
AKT2
AKT2 is a proto-oncogene that is amplified in 60% of pancreatic cancers. The protein product is an inhibitor of cell death (pro-apoptotic) proteins.
TP53
This tumor suppressor is critical in the life: death decision in abnormal cells. More than 50% of pancreatic cancers have a loss of function in this key gene.
SHH
This gene produces a protein that regulates nervous system development and may play a role in the formation of pancreatic cancer.
There has also been a recent discovery of pancreatic cancer stem cells (CSC) which have been shown to be involved in the initiation and recurrence of cancer due to their ability to evade current therapies. Research is underway to target these CSCs.15
Learn more about cancer stem cells
Treatment
The treatments for pancreatic adenocarcinoma are dependent on the stage at which it is diagnosed. Treatments include surgery, chemotherapy and radiation. The treatments chosen are dependent on the size of the tumor, its location within the pancreas, and stage of the cancer.16, 17
As our focus is on the biology of the cancers and their treatments, we do not give detailed treatment guidelines. Instead, we link to organizations in the U.S. that generate the treatment guidelines.11, 13
The National Comprehensive Cancer Network (NCCN) lists the following treatments for pancreatic adenocarcinoma:
- Chemotherapy
- Surgical Resection: surgical removal of the tumor (applicable to early stage tumors).
- Radiation Therapy: use of ionizing radiation to eliminate fast growing cancer cells.
- Palliative Care and Pain Management: Intrapleural/Celiac block is used to prevent pain associated with some cases of pancreatic cancer.
Learn more about cancer treatments
Information about clinical trials:
- General clinical trial information from CancerQuest
- Click here for information about clinical trials from the National Cancer Institute.
- Click here for information about clinical trials from Georgia Clinical Trials Online.
Pancreatic Cancer Resources
Risks for Pancreatic Cancer
Pancreatic Cancer Risk Factors (ACS)
Risks for Pancreatic Cancer (Mayo Clinic)
Cancer Center Treatments of America: Pancreatic Cancer Risk Factors
Detection and Diagnosis of Pancreatic Cancer
Winship Cancer Institute: Pancreatic Cancer Diagnosis and Staging Make an Appointment
What You Need To Know About: Pancreatic Cancer (2010)
Pancreatic Cancer Research Advances (NCI)
Pancreatic Cancer Treatments
Pancreatic Cancer Treatment (NCI)
Treatment: Pancreatic Cancer (Mayo Clinic)
Pancreatic Cancer Treatment (ACS)
Pancreatic Cancer Survivorship
Pancreatic Cancer Action Network
Pancreatic Cancer Survivorship
CTCA Survivorship Support for Pancreatic Cancer
Long Term Risks for Pancreatic Cancer Survivors
Long Term Effects of Pancreatic Cancer and Treatment
Symptoms and Side Effects of Pancreatic Cancer (Johns Hopkins Medicine)
Pancreatic Cancer Side Effects
International Pancreatic Cancer Resources
Pancreatic Cancer (Cancer Research UK)
NSW Pancreatic Cancer Council (Australia)
Pancare Foundation (Australia)
Australian Pancreatic Cancer Genome Initiative
Section Summary
Introduction
- Typically has a poor prognosis due to late diagnosis
- Successful treatment highly dependent on the stage of the cancer
- 4th overall cause of cancer death in the U.S.
Pancreatic Cancer Types
- 95% of pancreatic cancers are adenocarcinomas of the exocrine cells
- Other types include Sarcomas, Cystic Tumors, Acinar Cell Cancers, and Ampullary Cancers
Risk Factors
- Most pancreatic cancers are sporadic (non-familial)
- Rates slightly higher in men
- Risk factors include high BMI and diabetes
- Chronic inflammation plays a role (pancreatitis)
- Increased risk associated with smoking and smokeless tobacco use
Symptoms
- Very few symptoms in the early stages of the disease (many are unnoticeable)
- Symptoms include jaundice, weight loss, back/abdomen pain, steatorrhoea
Staging and Pathology Report
- Uses the T,N,M system to evaluate tumor size, lymph node involvement and metastasis
- Stages include: Resectable, Borderline Resectable, Locally Advanced Unresectable, Disseminated
Diagnosis
- Preoperative imaging done with CT scan or ultrasound to determine location and size of the tumor
- ERCP and biopsy may be used for further evaluation of the tumor
Pancreatic Cancer Tumor Biology
- Transformed cells contain a collection of mutations in key genes.
- Key genes include: K-Ras, AKT2, SHH, TP53, HER2/new, PTEN
- Altered genes may gain or lose function
- Cancer stem cells may play a role in tumor recurrence and metastasis
Treatment
- Treatment is dependent on the stage of the cancer
- Treatment possibilities include: Surgical Resection, Chemotherapy, Radiation Therapy, and Palliative Care and Pain Management.
- 1 American Cancer Society.Cancer Facts & Figures 2023. Atlanta: American Cancer Society. (2023). 取读于 从 https://www.cancer.org/research/cancer-facts-statistics/all-cancer-facts-figures/2023-cancer-facts-figures.html
- 2 Lee, Y. and Jun, H. "Glucagon-like peptide-1 receptor agonist and glucagon increase glucose-stimulated insulin secretion in beta cells via distinct adenylyl cyclases." International Journal of Medical Sciences. (2018); 15(6): 603-609. [PUBMED.]
- 3 Widmaier E. "Vander's Human Physiology 10th Edition." 2006. McGraw-Hill. NY
- 4 Ahn, DH and Bekaii-Saab, T. "Ampullary cancer: an overview" American Society of Clinical Oncology Educational Book. (2014); 112-115. [PUBMED]
- 5 AB Lowenfels, P Maisonneuve. Epidemiologic and etiologic factors of pancreatic cancer. Hematology/Oncology Clinics of North America. 2002; 16:1-16. [PUBMED]
- 6 AB Lowenfels and P Maisonneuve. Epidemiology and Prevention of Pancreatic Cancer. Japanese Journal of Clinical Oncology. 2004; 34(5): 238-44. [PUBMED]
- 7 Zhang, L., Sanagapalli, S., and Stoita, A. "Challenges in diagnosis of pancreatic cancer." World Journal of Gastroenterology. (2018); 24(19):2047-2060. [PUBMED]
- 8 Kikuyama, M., Kamisawa, T., Kuruma, S., Chiba, K., Kawaguchi, S., Terada, S., Satoh, T. "Early diagnosis to improve the poor prognosis of pancreatic cancer." Cancers (Base!) (2018); 10(2): 48. [PUBMED]
- 9 Banim PJ, Luben R, McTaggart A, Welch A, Wareham N, Khaw KT, Hart AR. Dietary antioxidants and the aetiology of pancreatic cancer: a cohort study using data from food diaries and biomarkers. Gut. 2012 Jul 23. [Epub ahead of print] [PUBMED]
- 10 American Cancer Society. Signs and Symptoms of Pancreatic Cancer. [https://www.cancer.org/cancer/pancreatic-cancer/detection-diagnosis-staging/signs-and-symptoms.html]
- 11abc National Comprehensive Cancer Network. "Pancreatic Adenocarcinoma." NCCN Clinical Practice Guidelines in Oncology V. 1.2008. (2007) [http://www.nccn.org/professionals/physician_gls/PDF/pancreatic.pdf]
- 12 American Cancer Society. Tests for Pancreatic Cancer. [https://www.cancer.org/cancer/pancreatic-cancer/detection-diagnosis-staging/how-diagnosed.html]
- 13ab R Freelove and AD Walling. Pancreatic Cancer: Diagnosis and Management. American Family Physician. 2006; 73(1):485-92. [PUBMED]
- 14 Ghaneh P, Costello E, Neoptolemos JP. "Biology and Management of Pancreatic Cancer." Gut (2007); 56:1134-1152 [PUBMED]
- 15 Smigiel, J., Parameswaran, N. and Jackson, M. "Targeting pancreatic cancer cell plasticity: the latest in therapeutics." Cancers (Base!) (2018); 10(1):14 [PUBMED]
- 16 Thomson BN, Banting SW, Gibbs P. Pancreatic cancer - current management. Australian Family Physician. 2006; 35(4): 212-17 [PUBMED]
- 17 American Cancer Society. Treating Pancreatic Cancer. [https://www.cancer.org/cancer/pancreatic-cancer/treating.html]
